Type of Stem Cell in Blood Vessels Might Treat Bleeding Disorders, Mice Study Shows
A newly identified class of stem cells in blood vessels, called vascular endothelial stem cells, were able to repair injured vessels and ease bleeding symptoms in a mouse model of hemophilia, researchers at Osaka University in Japan report, suggesting these cells may treat this bleeding disorder.
The vascular endothelial stem cells, or VESCs, were described in a study published in the journal Cell Stem Cell, titled “CD157 Marks Tissue-Resident Endothelial Stem Cells with Homeostatic and Regenerative Properties.”
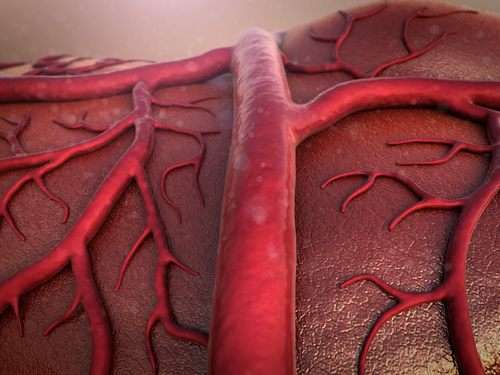
Vascular endothelial cells (ECs) are the major components of the inner surface of blood vessels. They are responsible for maintaining the function of blood vessels by promoting their repair when injured and forming new vessels when required.
Previous work by this research team suggested that a pool of endothelial cells could hold stem-cell potential, meaning they could transform into several cell subtypes as needed to sustain blood vessels. Until now, this endothelial stem-cell pool had not been identified.
“Our approach was to look for a cell-surface protein that is highly expressed in the endothelial stem-like population, but not in other ECs [endothelial cells],” Nobuyuki Takakura, the study’s senior author, said in a university news release. “This would theoretically allow us to isolate a homogeneous pool of candidate endothelial stem cells.”
The team found that a cell surface protein called CD157 appeared in high amounts in a small subset of ECs. These CD157-positive endothelial cells were scattered in different parts of the blood vascular system of adult mice, but only in large blood vessels and not in the capillaries (small blood vessels).
Based on the presence of CD157, the researchers isolated this specific pool of cells and transplanted them into mice with liver injury. The cells were found to not only proliferate in the mice but they also helped extensively to reconstitute the blood vessel network that was damaged. This striking effect was supported even when only a single CD157+ EC was transplanted.
“The results were more than we could have hoped for,” Takakura said. “A month after transplantation, the CD157-enriched cells generated fully functional portal veins, portal venules, sinusoids, hepatic venules, and arteries — essentially, every type of blood vessel found in a healthy liver.”
The potential of these CD157+ ECs was not restricted to the recovery of injured vessels but also helped to maintain healthy vessels in a sustained manner.
To further evaluate the therapeutic potential of these cells, the team also transplanted CD157+ cells collected from healthy mice into animals with hemophilia A.
The transplanted cells started to form new blood vessels in the liver, and the levels of FVIII — the clotting factor missing in hemophilia A — increased from 1 percent to more than 60 percent of the normal blood levels. This was accompanied by enhanced clotting activity.
“Our findings show that CD157-positive vascular endothelial stem cells give rise to a hierarchy of cell types that can repair vascular injury and maintain the normal blood vessel architecture,” Takakura said. “We believe these findings represent an entirely new way of thinking about how blood vessels are formed and, ultimately, how stem cells can be used to treat disorders related to blood vessel malfunction.”