Hemophilia A Patients with Transient Inhibitors to Factor VIII Can Usually Delay Therapy
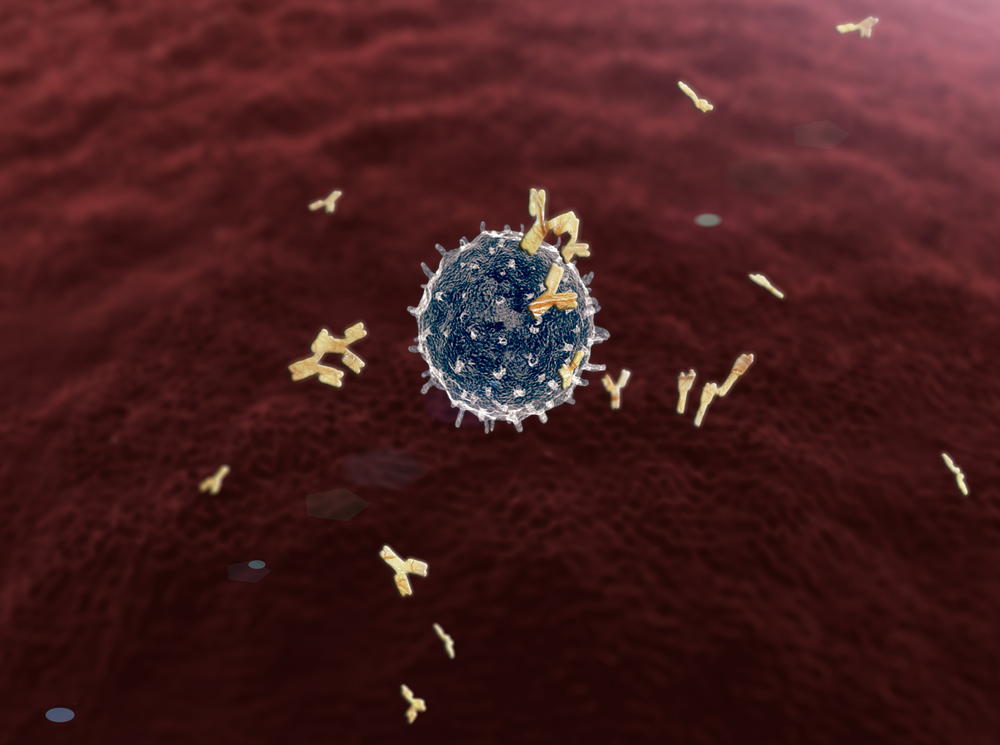
Hemophilia A patients who receive replacement therapies of factor VIII often develop inhibitors against factor concentrates which hinders the effectiveness of the therapy, increases disability, and reduces quality of life.
Although immune tolerance induction (ITI) can reduce inhibitors against factor VIII concentrates, the study “Long-term course of anti-factor VIII antibody in patients with hemophilia A at a single center,” published in Blood Research, suggests that therapy is not required in some cases because the inhibitor increase lasts for a short time and may disappear spontaneously.
Since the late 1960s, standard of care for hemophilia A has included replacement therapy using concentrates of the insufficient factors, particularly factor VIII which increases patient’s quality of life and life expectancy. But many patients experience complications such as the development of inhibitors that bind to factor VIII or factor IX molecules and neutralize clotting functions. The complication impacts approximately 30% of patients with severe hemophilia A and up to 7% of those with mild-to-moderate hemophilia A.
Inhibitors can be classified as either transient (short-lived) or persistent and can be eradicated with ITI therapy which reduces the inhibitors by up to 87%. However, symptoms that indicate need for treatment and when ITI should be administered have not been clearly defined.
To define eligible patients for ITI and when to start ITI, the researchers studied patients with hemophilia A registered at the Korea Hemophilia Foundation from 1991 through 2014. They classified the patients as those who developed transient or persistent inhibitors and then divided them according to the amount of inhibitors they exhibited — low, moderate, high, or very high.
Among the 1,634 hemophilia A patients, 100 developed persistent inhibitors and 250 developed transient inhibitors. Those with transient inhibitors were mainly in the low category and persisted for a median of 11 months. In the low, moderate, high, and very high groups, the median durations of inhibitor persistence were 10, 8, 13, and 19 months respectively, revealing that inhibitors at very high levels last significantly longer than those with low or moderate levels.
The researchers also found that study subjects with very high levels were also less likely to be transient. Only 21.7% of patients with very high inhibitor levels were transient, while 95.8%, 72.2%, and 52.4% of the low, moderate, and high groups became spontaneously inhibitor-negative (without ITI), respectively.
The findings suggest that ITI should be postponed for 11 months, which is when the majority of inhibitors (71.4%) in the study disappeared. Exceptions should be made for patients with very high levels of inhibitors who need ITI as soon as possible.