NovoSeven Linked to Low Rate of Dangerous Blood Clots in Review Study
Problematic thrombotic events are fairly rare in people using NovoSeven, among all types of bleeding disorders for which it is approved, including hemophilia, a review study shows.
The study, “Thrombotic events with recombinant activated factor VII (rFVIIa) in approved indications are rare and associated with older age, cardiovascular disease, and concomitant use of activated prothrombin complex concentrates (aPCC),” was published in the Journal of Blood Medicine.
NovoSeven (recombinant activated factor VII, by Novo Nordisk) is approved for the treatment of several types bleeding disorders, including Glanzmann’s thrombasthenia, hereditary and acquired hemophilia, and congenital factor VII deficiency.
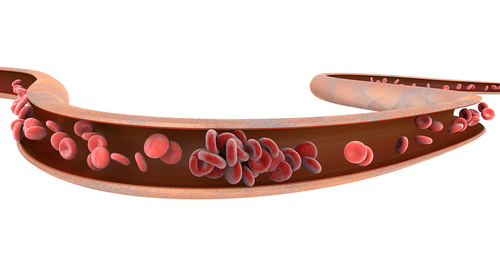
It works by setting off a molecular cascade that will allow for blood to clot. It has been shown to be an effective way to prevent bleeding in people with hemophilia; however, it carries the risk of causing serious thrombotic events, meaning blood clots that end up blocking the flow of blood in the circulatory system.
Novo Nordisk, in collaboration with U.S. researchers, reviewed data from clinical trials of NovoSeven, as well as from registries used to support its licensure and postmarketing surveillance, to determine how often thrombotic events occurred in people treated with NovoSeven. It was first approved for use in the U.S. in 1999.
Researchers analyzed data from 12,288 bleeding and surgical episodes reported. Among these, 21 thrombotic events occurred in 18 patients, representing an overall incidence rate of 0.17%. Divided according with hemophilia type, thrombotic event rates were 0.11% for congenital hemophilia with inhibitors, 0.82% for factor VII deficiency, 0.19% for Glanzmann’s thrombasthenia, and 1.77% for acquired hemophilia.
Further analyses revealed that the biggest risk factor for an thrombotic event was older age (65 or older), with over a quarter of the events (28.6%) occurring in elderly patients. Other risk factors included the use of activated prothrombin complex concentrates (aPCC) and the presence of broadly defined heart disease, both of which were present in 17.8% of all events.
These findings suggest that people with hemophilia who fall into any of these categories should be followed carefully by their healthcare providers if using NovoSeven to prevent a potentially harmful adverse event.
Other conditions thought to be potential risk factors — such liver disease, sepsis (generalized infection), pregnancy, very young age (infancy), and crush injuries — were rare among those who experienced a thrombotic event, or not reported at all.
This finding is noteworthy because it suggests that factors that increase the risk for thrombotic events are likely different in people with or without bleeding disorders.
“For more than a decade, risk factors typically associated with thrombosis in patients without an underlying bleeding disorder were included in the [prescription information] as warnings,” the researchers wrote.
“However, the present analysis suggests that older age, cardiac and cardiovascular disease (beyond atherosclerosis only), and concomitant use of aPCC are the most common associated risk factors for thrombosis among patients with hemophilia.”
Overall, this study demonstrates that thrombotic events in people using NovoSeven are “very low,” and highlights the need for understanding clotting risks specifically in people with bleeding disorders.
One of the study’s four authors is an employee of Novo Nordisk.