Bleeding, blood clot-related events in US tied to acquired hemophilia
Researchers studied 1,450 patients admitted to hospital between 2016 and 2019
About 30% of people hospitalized due to acquired hemophilia have a bleeding event, while 17% report a thrombotic, or blood clot-related complication, such as stroke and deep vein thrombosis, a nationwide U.S. study finds.
Patients ages 65 years and older, and those with thrombotic events were more likely to die during a hospitalization. Also, about a third were readmitted within 30 days of being discharged, mainly due to bleeding events and infections.
“This large collection of [acquired hemophilia] admissions and readmissions on a nationwide scale has generated a valuable pool of data, helping to characterize the clinical outcomes and healthcare utilization of this otherwise rare [blood condition],” the researchers wrote. The study, “Acquired (Autoimmune) Hemophilia: Demographics, Outcomes, and Readmissions,” was published in Blood Vessels, Thrombosis & Hemostasis.
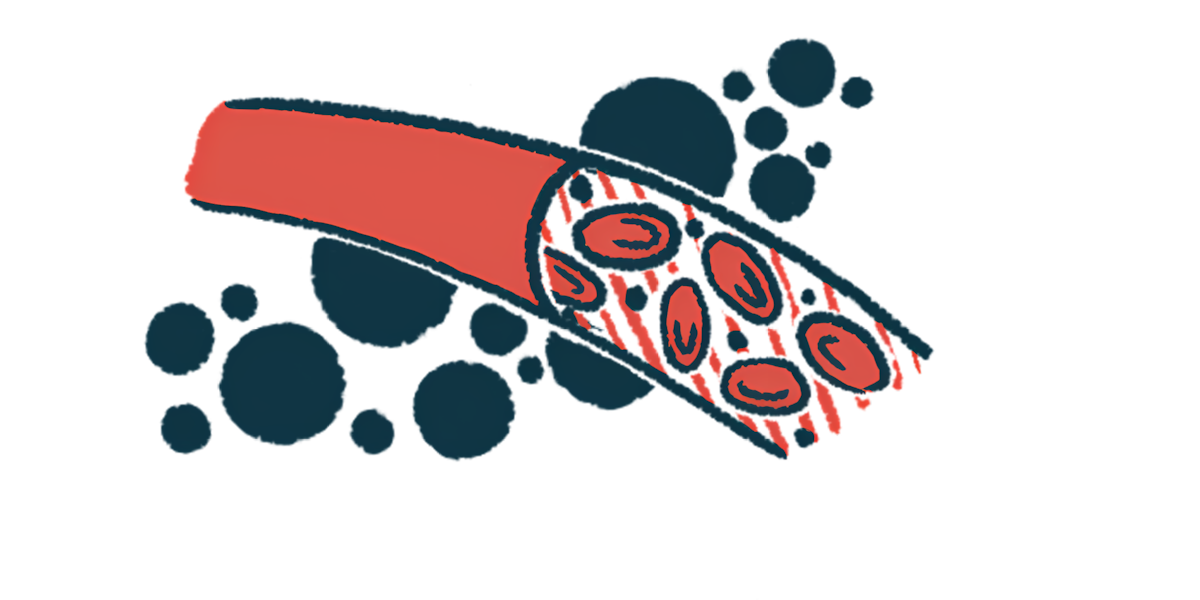
While most types of hemophilia are caused by genetic mutations, acquired hemophilia has an autoimmune origin and arises when the immune system mistakenly attacks a blood clotting factor, preventing it from functioning normally. In most cases, it targets factor VIII (FVIII), the clotting protein missing or faulty in hemophilia A.
In more than half the patients, the disease is idiopathic, or has an unknown cause, while in the other half, it’s associated with other conditions, including autoimmune disorders, cancer, infections, or certain medications.
Treating acquired hemophilia is focused mainly on keeping bleeds under control and suppressing the immune system to reduce the production of the self-reactive antibodies that target clotting factors.
A better look at acquired hemophilia
“Though there have been significant developments in the treatment aspects, not much literature exists on the epidemiology and outcomes of these treatments on a larger population basis,” wrote researchers in the U.S. who conducted a retrospective study using the Nationwide Readmissions Database, which contains information on hospital discharges and readmissions.
A total of 1,450 patients were admitted to the hospital for acquired hemophilia between 2016 and 2019. More than half were men (55.4%), with a median age of 73 when they were admitted. The median length of their hospital stay was seven days.
About 21% had an underlying solid tumor, while 13.5% had an autoimmune disease, and 3.9% had blood cancer. Autoimmune diseases were significantly more frequent in women (22.2% vs. 6.4%) and in those 65 years and older (15.1% vs. 8.5%). No differences in cancer prevalence were seen between gender and age groups.
Almost a third of the patients had a bleeding event. Other complications during hospitalization included heart attack (9.5%), venous thromboembolism, which is when a blood clot blocks blood flow in veins (4.4%), stroke (2.5%), brain hemorrhage (1.5%), and widespread formation of blood clots (1.2%). During their hospitalization, about a quarter of the patients received blood transfusions and 5.4% required invasive ventilation.
Overall, 101 patients (7%) died during their inpatient stay, with higher mortality rates seen in older patients (8% vs. 3%) and in those who’d had a stroke (34.4% vs. 6.3%) or venous thromboembolism (19.6% vs. 6.4%). The median time to death was nine days. The presence or absence of autoimmune conditions or cancer had no effect on mortality rates.
Of the 1,349 patients discharged, 371 (27%) were readmitted within 30 days. This occurred more frequently in those who had an underlying autoimmune condition (35.5% vs. 23.3%). Hospital readmissions lasted a median of seven days, and 10.8% of the patients died.
The most common causes for readmission were infections (30.8%), followed by bleeding (28.2%). Other reasons included heart problems (7.6%), cancer (5.7%), bone fractures (5.6%), and neurologic events (4.6%).
Median hospitalization costs were about $113,000 in first admissions and readmissions.
“These results highlight the complex challenges in managing this disease. High infection rates emphasize the toxic effects of immunosuppressive therapy, while higher bleeding rates demonstrate inadequate inhibitor clearance,” the researchers wrote.