Saliva protects against mouth and throat bleeds in hemophilia A: Study
About 90% of bleeds affect joints, but oropharyngeal bleeds are rare
Written by |

Small vesicles in the saliva of people with severe hemophilia A may explain why these patients rarely have bleeds in their mouth and throat. The vesicles contain a protein complex that’s able to induce blood coagulation in these patients, thereby reducing bleeding.
The findings may help “develop innovative approaches for research and potentially also for the targeted treatment of patients,” Johannes Thaler, MD, PhD, at Medical University of Vienna in Austria and the study’s lead author, said in a university news story.
The study, “Saliva of persons with hemophilia A triggers coagulation via extrinsic tenase complexes,” was published in Blood.
Hemophilia is a genetic disease where blood doesn’t clot properly because a clotting factor is either faulty or missing, resulting in excessive bleeding and bruising. In hemophilia A, the faulty or missing clotting factor is factor VIII (FVIII). Up to 90% of all bleeds in hemophilia A patients affect the joints, whereas other types of bleeds, including those in the mouth and throat, called oropharyngeal bleeds, are rare.
It has’t been known why this happens until a team led by researchers at the Medical University of Vienna showed that the saliva of people with hemophilia A naturally triggers blood coagulation. They found their saliva contains tiny extracellular vesicles (EVs) that carry two coagulation factors — tissue factor (TF) and activated factor VII (FVIIa) — that are capable of triggering blood clotting. Both proteins are organized in a complex structure called tenase complexes, which can initiate the coagulation cascade when they come into contact with blood.
‘Empowering’ coagulant in hemophilia A
In their first experiments, the researchers collected saliva samples from people with severe hemophilia A and added it to blood samples that lacked FVIII. This significantly accelerated blood clotting and led to the production of thrombin, an enzyme that causes the blood to clot, as well as the formation of activated factor X (FXa), an important player in the coagulation cascade that’s responsible for generating thrombin. When saliva wasn’t added, the blood didn’t clot.
While previous studies showed that the coagulation activity of saliva was solely due to the presence of EVs exposing tenase complexes, this had “never been studied in saliva derived from persons with hemophilia A.”
In another experiment, the researchers used saliva samples that contained fewer EVs. Here, the formation of FXa was significantly reduced. The findings confirmed that the factors that triggered blood coagulation in saliva are present in EVs.
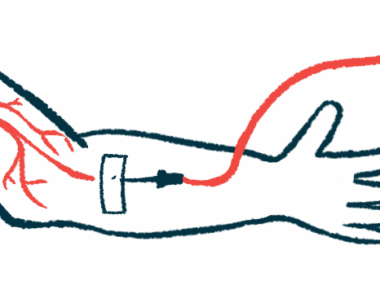
They then analyzed saliva samples obtained before and after patients received vein infusions of FVIII replacement therapy, the standard treatment for hemophilia A to prevent or reduce the frequency of bleeds. They confirmed the blood clotting-inducing potential of saliva was unaffected by treatment.
The researchers also analyzed the rates and sites of bleeding for 12 months from six patients with severe hemophilia A who received treatment only when they’d had a bleed, which is known as on-demand treatment.
From 105 bleeding episodes, only 21 were mucosal bleeds, with 19 being oropharyngeal bleeds. The remaining mucosal bleeds affected the gastrointestinal lining and the urinary tract. All the oropharyngeal bleeds stopped spontaneously without replacement therapy, while the other mucosal bleeds required treatment. Most of the bleeds (66%) across all the patients occurred in the joints and all required treatment.
The researchers said the findings “contribute to our understanding of the bleeding in hemophilia A, and noted that “informing persons with hemophilia A not only about what their coagulation system cannot do, but also what it can do, may be experienced as empowering.”