FVIII Prophylaxis Early in Life Improves Joint Outcomes in Hemophilia A, Study Shows
Written by |
Starting factor VIII (FVIII) preventive therapy before the age of 2.5 years improves joint outcomes in young adults with hemophilia A compared to starting treatment later in childhood, a clinical trial shows.
The study, “ Young adult outcomes of childhood prophylaxis for severe hemophilia A: results of the Joint Outcome Continuation Study,” was published in the journal Blood Advances.
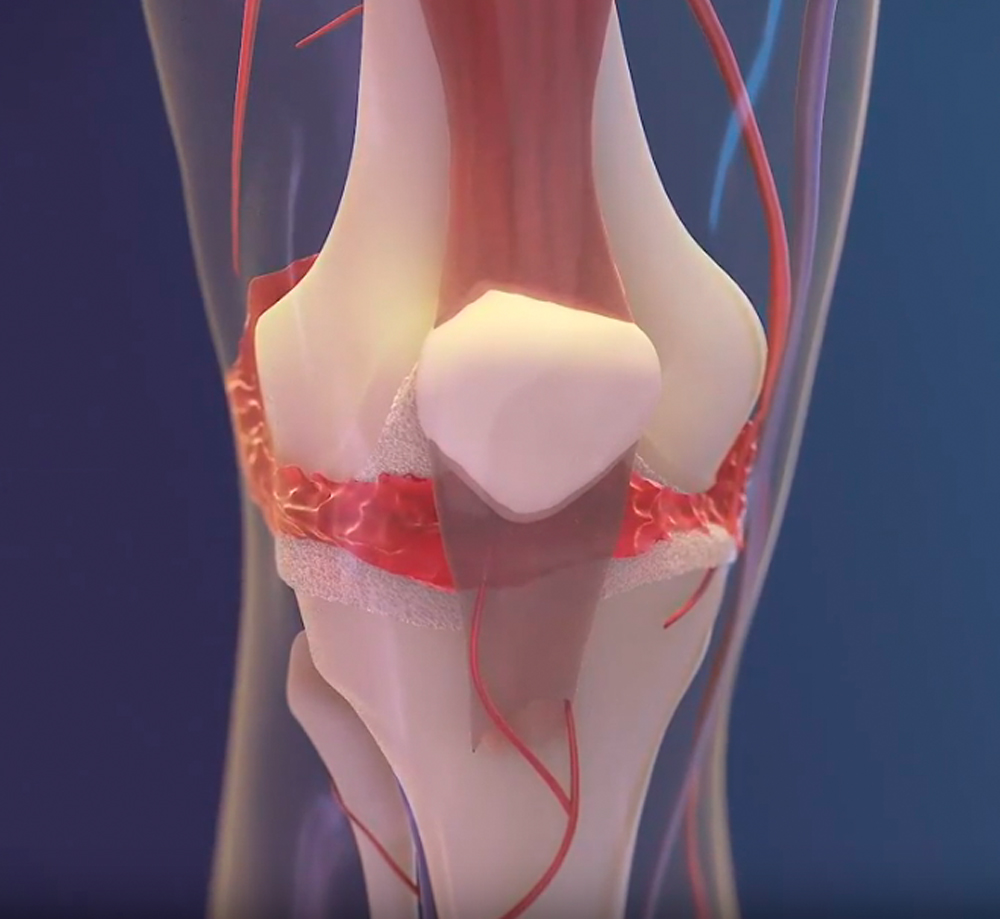
Joint bleeding in people with severe hemophilia A is caused by small traumas, and leads to arthropathy (joint disease), pain, and diminished quality of life.
Severe hemophilia A occurs when the levels of FVIII, an essential blood clotting protein, drop to less than 2%. FVIII replacement has been a standard preventive (prophylactic) therapy, but implementing such treatments worldwide has been limited due to high costs, the need for into-the-vein administration, and doubts concerning efficiency.
The Joint Outcome Study (JOS) (NCT00207597) was a clinical trial that tested whether the starting age of preventive FVIII therapy influenced the progression of joint disease in boys with severe hemophilia A. Results showed that starting preventive treatment before age 2.5 led to better joint outcomes at age 6 than on-demand treatment with FVIII for bleeding.
These results, and because prophylaxis is not able to reverse osteochondral damage (one that affects the cartilage of a joint and the bone underneath), the World Federation of Hemophilia recommended FVIII therapy to start before age 3 and prior to joint bleeding.
Following the JOS study, adoption of FVIII prophylaxis was encouraged for all participants, and the Joint Outcome Study Continuation study (JOS-C) followed these patients through adolescence. Researchers then compared long-term joint outcomes regarding the age at beginning of treatment.
JOS-C (NCT01000844) enrolled 37 of the 65 boys who had participated in JOS originally. Participants were enrolled from 11 U.S. sites, between January 2010 and September 2015.
Fifteen patients were part of the early prophylaxis group and 18 were in the delayed prophylaxis (or episodic) group. The four remaining participants developed high-titer FVIII inhibitors (neutralizing antibodies) and were analyzed separately.
Treatment initiation occurred at a mean age of 1.3 years in the early prophylaxis group, and of 7.6 years in participants with delayed prophylaxis. This group included three participants starting prophylaxis after age 10.
Eight participants (44%) in the delayed group were prescribed high doses of prophylaxis within 40 to 50 units per kilogram (U/kg), while only three patients (20%) on the early prophylaxis group had similar dosing.
The researchers observed that at age 18 the risk for osteochondral joint damage was 6.3 times higher in the delayed prophylaxis group compared to the early group, as 77% of participants on delayed prophylaxis had such damage (as found with MRI) compared to 35% of those on early treatment.
In addition, the annualized bleed and joint bleed rates from birth to age 18 in the early prophylaxis group were one-third of the rates in the delayed group. A significant reduction in bleeding rates also was observed when comparing the period between beginning prophylaxis and age 18.
The extended MRI (eMRI) score evaluates each joint in a nine-point scale for soft tissue damage and a 36-point scale for osteochondral damage, where higher scores correspond to more damage. Results showed that the eMRI 6-joint total score was 7.8 for the early group and 13.8 for the delayed group.
Likewise, physical examination with the Colorado Pediatric Joint Assessment Scale (CPJAS) also showed more severe damage in the delayed group.
Sports and physical activity analysis of 24 participants without inhibitors — 12 early prophylaxis and 12 delayed prophylaxis — revealed that 66% of patients playing moderate or high risk sports showed no osteochondral damage in the early group, while 37.5% of the delayed group had no signs of joint damage.
No significant differences in any domain were found between the two groups in the Haemo-QOL quality-of-life questionnaires. Yet, the researchers said that Haemo-QOL have low sensitivity to detect differences in quality of life of generally healthy individuals.
“In severe HA [hemophilia A], early initiation of prophylaxis provided continued protection against joint damage throughout childhood compared with delayed initiation, but early prophylaxis was not sufficient to fully prevent damage,” the scientists wrote.
Overall, the findings support the recommendation by the World Federation of Hemophilia for early treatment initiation and before first joint bleed.
In recent years, extended half-life FVIII replacement, non-factor based therapies — like Hemlibra (emicizumab) — have significantly improved hemophilia treatment. However, predictions of long-term outcomes of recent treatments are still not possible.
The findings from JOS-C provide a reference that can be used to compare new therapies, the team said.


