Hemophilia gene therapy Beqvez reduces bleeds in Phase 3 trial
Patients saw about 3 times fewer bleeding episodes vs. prophylaxis
Written by |
Hemophilia gene therapy Beqvez (fidanacogene elaparvovec), marketed as Durveqtix in the European Union, results in stable production of factor IX (FIX), the clotting protein that is missing or faulty in hemophilia B, leading to about three times fewer bleeding episodes compared with prophylaxis, or preventive treatment, with regular infusions of FIX.
That’s according to final data from BENEGENE-2 (NCT03861273), the Phase 3 study that supported this year’s approval of Beqvez as a one-time treatment for adults with moderate to severe hemophilia B in the U.S. Beqvez is also approved in Canada and the European Union to treat moderately severe to severe hemophilia B.
“What we saw from patients in this study was that within a few days of receiving the gene therapy infusion, it took root, and their bodies started making factor IX for the first time in their lives,” Adam Cuker, MD, clinical director of the Penn Blood Disorders Center at the University of Pennsylvania and the study’s first author, said in a university news story.
This suggests that the gene therapy could move patients away from regular infusions toward a more sustainable treatment option. “We always want to be careful about using the word ‘cure’ especially until we have longer follow-up data, but for many of these patients, it’s been life changing,” Cuker said.
The study, “Gene Therapy with Fidanacogene Elaparvovec in Adults with Hemophilia B,” was published in The New England Journal of Medicine. It was supported by Pfizer, the company that markets the gene therapy.
Hemophilia gene therapy delivered to liver cells
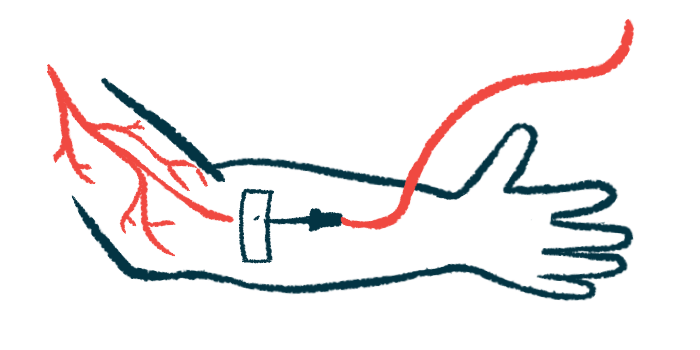
In hemophilia B, blood cannot clot properly, and even minor injuries can lead to excessive bleeding. Treatment usually consists of the regular administration of infusions of a version of FIX, the clotting protein that’s missing or is faulty in patients with the disease, but this can be time-consuming and costly.
Given as a single infusion directly into the bloodstream, Beqvez is designed to deliver a highly functional version of the gene encoding FIX, packaged aboard a viral vector, to cells in the liver. Once the gene therapy is taken up by liver cells, the cells can use its instructions to produce the clotting protein on their own.
The BENEGENE-2 study involved 45 men with moderately severe to severe hemophilia B who had been receiving regular infusions of FIX as part of a six-month lead-in study (NCT03587116). All tested negative for neutralizing antibodies against the viral vector that carries Beqvez, which could limit its delivery to the liver.
A single dose of Beqvez was generally well tolerated and caused the overall annual bleeding rate to drop by 71%, from a mean of 4.42 bleeding episodes per year in the lead-in study to 1.28 after treatment with Beqvez (month 3 to month 15 following infusion). The annual rate of treated bleeds also dropped by 78% in the same period, from a mean of 3.34 bleeding episodes per year in the lead-in study to 0.73 after treatment with Beqvez.
These reductions in annual bleeding rates were also associated with a decrease of approximately 92% in the mean annual infusion rate and total FIX consumption.
The proportion of patients who remained free of bleeds also increased, from 29% during prophylaxis to 64% after the gene therapy, as did the percentage of those who remained free of bleeds that required treatment, which rose from 36% to 73%.
At the 15-month mark, mean FIX activity was at 26.9%, indicating a sustained production of the clotting protein. However, some side effects were reported, with 62% of patients needing glucocorticoids to manage elevated liver enzymes, a sign of liver damage.
Despite these side effects, there were no severe reactions related to Beqvez, such as serious allergic reactions or clotting problems. None of the patients developed inhibitors against FIX.
“We hear from people born with hemophilia that — even if their disease is well-managed — there’s this burden that’s always in the back of their mind,” Cuker said. “The frequent infusions, the cost of treatment, the need to plan for infusions when traveling, what happens if they do experience a bleed, and so on, is always there. Now that we have patients who were treated on this study and are essentially cured of their hemophilia, they’re telling us about realizing a new, ‘hemophilia-free state of mind.’ As a physician, it’s amazing to see my patients so happy with their new reality.”