Immune Deficiencies With FVIII Inhibitors Evident, But Can Be Restored
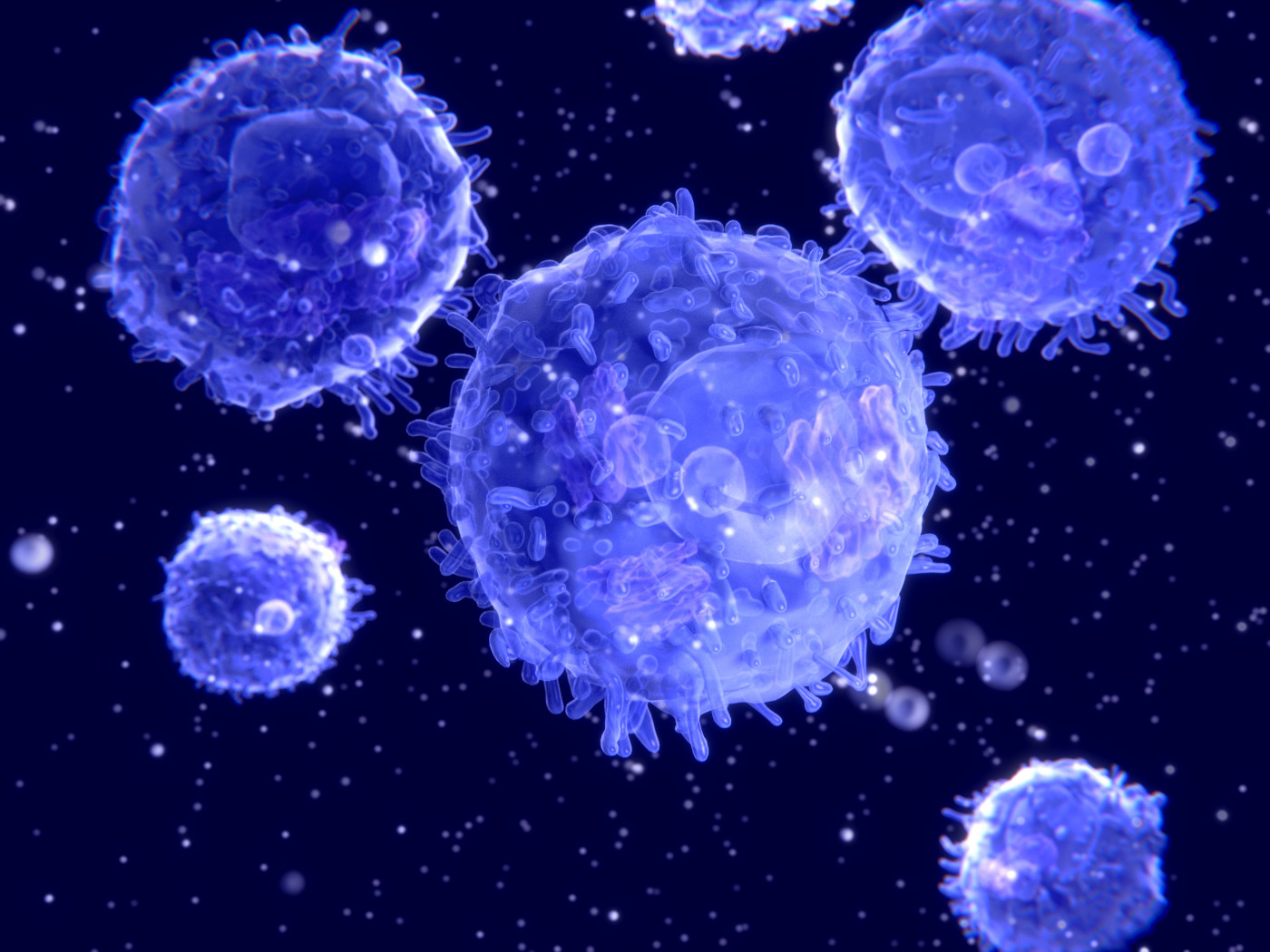
Hemophilia A patients with factor VIII (FVIII) inhibitors show deficiencies in regulatory B- and T-cells — immune cells that typically dampen immune and inflammatory responses — but their levels can be restored with successful immune tolerance induction (ITI), a study shows.
These findings shed light on how ITI — given to eradicate inhibitors in patients — works in the body, and support evidence linking the presence of FVIII inhibitors with a reversible deficiency in peripheral immune tolerance. As such, study results may also help to identify new targets for reinstating immune tolerance, its researchers noted.
The study, “Role of Regulatory Cells in Immune Tolerance Induction in Hemophilia A,” was published in the journal HemaSphere.
A standard treatment for hemophilia A, FVIII replacement therapy supplies patients with lab-made FVIII, the blood clotting factor they are missing. However, around a third of patients develop inhibitors, or neutralizing antibodies, against the delivered FVIII, negating its effectiveness.
ITI is the only known way of effectively removing FVIII inhibitors. It involves giving a person high doses of FVIII over a period of time, until the body is trained to recognize the product without mounting an immune response against it — a phenomenon known as immune tolerance.
However, “the working mechanism of ITI is incompletely understood as few studies thus far addressed FVIII-induced immunological changes during ITI,” the researchers wrote.
To clarify these mechanisms, a team of researchers in the Netherlands analyzed the levels of immune cells and markers associated with immune tolerance in hemophilia A patients with and without FVIII inhibitors, before and after ITI.
The first analysis included 65 patients: 28 without FVIII inhibitors, 20 with inhibitors, and 17 who had inhibitors in the past (ex-inhibitor patients). Neutralizing antibodies resolved spontaneously in three of these patients, and through use of ITI in the 14 others.
Immune changes before and after ITI were also assessed in 12 other hemophilia A patients with inhibitors, and compared with those of 36 inhibitor-negative patients. Of note, ITI was given for a median duration of 1.6 years, and led to the complete eradication of FVIII inhibitors in 10 of the 12 (83.3%).
All patients were treated at the hemophilia treatment center of the University Medical Center Utrecht, and their blood samples were collected between 2001 and 2018.
Analyzed immune cells included regulatory B-cells (Bregs), regulatory T-cells (Tregs), and myeloid-derived suppressor cells (MDSCs). Tolerance markers evaluated were programmed cell death protein 1 (PD1), programmed death-ligand 1 (PD-L1), inducible T-cell costimulator (ICOS), and cytotoxic T-lymphocyte-associated protein 4 (CTLA4).
Of note, Bregs and Tregs keep the body’s immune response in check by regulating or suppressing other immune cells. They can control, or regulate, the immune response not only to foreign molecules, but also to the body (self) — which is key in preventing autoimmune reactions.
While MDSCs have been mostly studied in cancer, they have also been described as being involved in tolerance induction in autoimmune diseases.
Results showed that inhibitor-positive patients had a significantly lower frequency of Bregs (3.2%), compared with inhibitor-negative (5.9%) and ex-inhibitor patients (8.9%). No significant differences in the levels or frequencies of Tregs and MDSCs were observed among these groups.
Among tolerance markers, CTLA4 — present both on effector T-cells, which promote immune responses, and on Tregs — was the only one found to be significantly different among the groups.
Particularly, CTLA4 levels were significantly lower in patients with FVIII inhibitors relative to the inhibitor-negative group. Similar, but non-statistically significant, trends were observed for PD1, ICOS, and PD-L1.
Notably, the data also highlighted that FVIII inhibitor eradication was significantly associated with an increase in the frequencies of Bregs and Tregs, and in the levels of tolerance markers CTLA4 and PD1 on Tregs, when compared with pre-ITI measures.
This was in contrast with the stable levels of immune cells and tolerance markers observed over time in patients without inhibitors.
“We found the lowest frequency of immunoregulatory cells and markers, in particular of Bregs and CTLA4 on T-cells, in inhibitor patients, with evidence for reversal during ITI, supporting the role of these immunoregulatory components in restoration of tolerance to FVIII,” the researchers wrote.
“These results suggest that an existing anti-FVIII immune response is associated with deficits in peripheral tolerance mechanisms, which can recover during the course of ITI,” they added.
Researchers hypothesized that Bregs may drive immune tolerance restoration by producing IL-10, an anti-inflammatory molecule known to support the generation and maintenance of Tregs, but emphasized that further studies are needed to confirm this.
Future research is also needed to validate these findings, and to “exploit the identified key immunoregulatory cells and markers towards the development of improved ITI protocols,” the team wrote, noting that IL-10 and CTLA4 may be good therapeutic candidates to help restore immune tolerance.