Insurer Highmark Forges New Hemophilia Partnership Focused on Treatment, Management
Written by |
As part of a new partnership focused on hemophilia treatment and management, members of insurer Highmark will receive medication exclusively from Option Care Health, Soleo Health, and the Hemophilia Center of Western Pennsylvania.
The collaboration that begins in January is aimed at keeping down costs associated with medication waste and fraud. It also aims to ensure that its 190 members with hemophilia get their medicine from companies that meet robust performance standards.
An independent licensee of the Blue Cross Blue Shield Association, Highmark spends roughly $80 million annually on hemophilia care, about 90% of that in pharmacy costs.
“The organizations in our high-performance hemophilia partnership are true centers of excellence in the treatment of this complex, chronic condition,” Ned Finn, Highmark’s director of specialty pharmacy services, said in a press release. “By partnering with these organizations, we are able to obtain hemophilia drugs for our members at a competitive rate while establishing new performance guarantees and oversight protocols for providers. Our members will work with organizations that possess exceptional knowledge of hemophilia, and will receive the right drugs and dosage at the right time.”
The result, he added, will be a higher level of member care and prospective cost savings.
Kurt Spear, vice president of Highmark financial investigations and provider review, said that over the last year, the company identified and blocked several attempted fraud, waste and abuse (FWA) schemes.
“Highmark understands that the risk of FWA associated with prescription drugs, including those used to treat hemophilia, are high,” he said. “Our new network is another step to mitigate these risks for our customers.”
The partnership aligns with the insurer’s Hemophilia Member Care Program, which it introduced this year. Employing a high-tech, multidisciplinary approach, the program identifies hemophilia patients, helps them better understand their condition, and develops an individualized care plan. After identifying members based on risk, the hemophilia care management team begins its work. The team consists of a nurse, pharmacist, physician, and other clinicians.
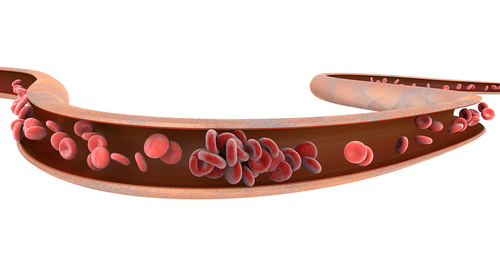
A national leader in treating blood disorders, Option Care Health provides specialized intravenous (into-the-vein) infusion of clotting factors — which hemophilia patients do not have — that control bleeding. It has access to the different types of clotting factors associated with the various types of the disorder.
“Highmark chose to partner with Option Care Health because of the extraordinary care we provide to patients as well as our rigorous performance standards and ability to control drug waste and costs while still delivering excellent outcomes,” Rich Denness, chief strategy officer for Option Care Health, said in an press release. “The health plan recognizes that we will provide their members who have been diagnosed with hemophilia the highest-quality personalized care to help manage this complex and challenging condition.”
In November, Highmark announced it was partnering with pharmacy and infusion services provider Soleo Health to help it care for members with hemophilia. Soleo was chosen for its clinical expertise and data-reporting capabilities, Highmark said.
The Hemophilia Center of Western Pennsylvania provides comprehensive multidisciplinary care for Highmark members with hemophilia and other inherited coagulation disorders. Its clotting factor program was established in 2000 to complement the center’s other comprehensive care services.
“Managing hemophilia can be a complicated process,” Finn said. “Our goal is end-to-end treatment for our members that removes barriers to better health and allows them to enjoy the highest quality of life possible.”
According to the Centers for Disease Control and Prevention, hemophilia occurs in about one of every 5,000 male births.


