FVIII infusion resolves rare GI bleeding in hemophilia A patient
Intramural hematoma occurs less often in hemophilia B, literature reveals
A 48-year-old man with severe hemophilia A developed a rare intramural hematoma with blood leaking into one of the layers of the intestine wall that was successfully treated with an early infusion of the missing blood clotting factor, a recent case report described.
Prophylactic treatment prevented its recurrence. A review of the literature suggests intramural hematoma, although rare, affects mostly hemophilia A patients.
“We believe that our case report with a literature review will be clinically helpful for physicians to manage better the rare risky intramural hematoma in [people with hemophilia],” the researchers wrote in “Intramural Hematoma of Gastrointestinal Tract in People with Hemophilia A and B,” which was published in the Journal of Clinical Medicine.
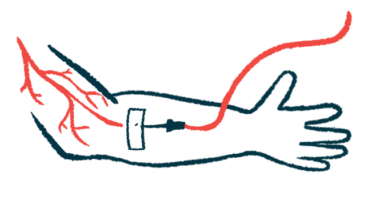
Hemophilia is a blood disorder that affects the ability to form blood clots to prevent excessive bleeding. In hemophilia A, this clotting impairment is caused by the lack of a specific protein, called factor VIII (FVIII). In hemophilia B factor IX (FIX) is missing.
Both hemophilia A and B feature spontaneous bleeding episodes in different parts of the body, including joints, muscles, and the gastrointestinal (GI) tract. Bleeding into the GI lumen — the space inside the digestive tract where food and fluids pass through — is a common hemophilia complication reported in 10-25% of patients.
Intramural hematoma, when blood leaks into the submucosal layer, an intermediate tissue layer between the mucosa and the external wall of the digestive tract, is rare.
Researchers at the Taipei Medical University Hospital, Taiwan described the case of a 48-year-old man with severe hemophilia A who developed a spontaneous intramural hematoma of the jejunum, the middle part of the small intestine.
Treating intramural hematoma in hemophilia A
He’d been treated with on-demand FVIII infusions for more than 40 years and was being followed at the researchers’ hospital for 15 years. His clinical history included severe joint disease and a resolved hepatitis C virus infection.
In June 2019, he went to the emergency room complaining of generalized abdominal pain lasting for three days, accompanied by reduced appetite and nausea, but no fever. A day before being admitted, he had tar-colored stools, a sign of upper GI bleeding.
Lab work showed a high white blood cell count, especially of neutrophils, and high levels of C-reactive protein, a marker of generalized inflammation. Hemoglobin levels and platelet counts were normal, but his activated partial thromboplastin time (aPTT), a test that measures the time it takes for blood to clot, was longer than normal (146.3 seconds; normal range, 32-45 seconds).
The man had a CT scan of his abdomen, which revealed a thickening of the bowel wall in the jejunum, consistent with an intramural hematoma. Ascites, an abnormal accumulation of fluid, surrounding the spleen also was seen.
He was placed on bowel rest and was treated with Eloctate, an extended half-life (EHL) FVIII product. FVIII activity levels were maintained at 40% with 1,000 international units (IU) of Eloctate every 12 hours. He also received antibiotics to prevent infections.
His pain eased and tarry stools resolved. The Eloctate dose was gradually tapered (1,000 IU daily) and the man was started on a clear liquid diet and later transitioned to a soft diet.
After six days in the hospital, he was stable and discharged without complications. He refused preventive treatment with FVIII, despite medical advice.
He developed similar symptoms nearly three months later, suggesting the intramural hematoma had recurred. No tarry or bloody stools were seen, but he hadn’t had a bowel movement in the three days. A CT scan confirmed an intramural hematoma, causing a partial bowel obstruction.
He was treated with 2,500 IU of Eloctate every 12 hours to maintain FVIII levels at around 80%. An enteroscopy, which examines the small intestine, ruled out a tumor in the jejunum.
His condition stabilized after nine days and he was discharged without any complications. He was placed on 4,500 IU of Eloctate once a week as a prophylactic and had no recurrences for more than three years.
The researchers reviewed the literature, gathering data from 79 reported cases of intramural hematomas with hemophilia — 62 occurring in hemophilia A patients, four with hemophilia B, and 13 with an unknown hemophilia type.
They were more frequently seen in the small intestine (34 cases) and the colon (17 cases). The intramural hematoma mortality rate was 12.2%, with higher rates seen in children (23.3%) than adults (4.9%).
Intramural hematoma of the GI tract is rare in hemophilia, but this case report suggests “early conservative therapy with CFCs [clotting factor concentrates] infusion should be the first-line therapeutic option,” with surgery “reserved for complicated cases,” the researchers wrote.