Gene therapy for hemophilia
Last updated Oct. 31, 2025, by Marisa Wexler, MS

Hemophilia is a bleeding disorder that is caused by genetic mutations in most cases. Gene therapy is an approved strategy for treating hemophilia that works by delivering a healthy version of the gene whose defect causes the disease.
Gene therapies are approved by the U.S. Food and Drug Administration (FDA) for both hemophilia A and hemophilia B, and investigational gene therapies are in development.
These treatments hold the potential to provide long-lasting symptom management and life-quality improvements with a single infusion, though they also carry risks of side effects. Because gene therapies for hemophilia are still relatively new, much about their long-term impact is not yet known.
How gene therapy works for hemophilia
Hemophilia is mainly caused by mutations in genes that provide instructions to make proteins that help blood to clot. Mutations in the F8 gene that encodes clotting factor VIII are the underlying cause of hemophilia A, while mutations in the F9 gene that encodes clotting factor IX are the root cause of hemophilia B. In either case, mutations lead to reduced clotting factor activity, meaning that blood cannot clot properly, ultimately leading to the disease’s hallmark symptoms of easy and prolonged bleeding.
Traditional treatment for hemophilia involves factor replacement therapy, where a version of the missing or faulty protein is infused into the bloodstream. A drawback of this approach is that patients with hemophilia generally require regular infusions over the course of their lives, which can be burdensome and expensive. Nonfactor hemophilia treatments are also available, but these generally require lifelong use too.
The basic concept behind gene therapy for hemophilia is to deliver a healthy version of the mutated gene to liver cells, which serve as the body’s main producers of clotting proteins. The goal is to restore the body’s ability to produce a functional version of the missing or faulty clotting factor protein and ultimately normalize blood clotting to minimize bleeding symptoms. Theoretically, the main advantage is that once the therapeutic gene is administered, liver cells can produce the clotting protein indefinitely. As such, gene therapy may allow for long-term symptom control after a single infusion, reducing the need for other treatments.
Available gene therapies use viral vectors to deliver their genetic payload to cells. These vectors are basically viruses engineered to deliver a therapeutic gene instead of causing a harmful infection. Approved gene therapies specifically use vectors derived from adeno-associated virus (AAV). This virus is often used as a platform for gene therapies because it is easy to work with in a lab and generally doesn’t cause serious illness in people.
Apart from AAV-based gene therapy, other approaches are being explored, such as CRISPR/Cas9, a gene-editing technology that can be used to alter the genetic code within a cell. These other hemophilia gene treatments are still in early stages of development.
Current gene therapy approaches for hemophilia
In the U.S., the two FDA-approved gene therapy options for hemophilia are:
- Roctavian (valoctocogene roxaparvovec-rvox), a gene therapy for hemophilia A that is approved for adults with severe disease who don’t have detectable antibodies against the therapy’s viral vector
- Hemgenix (etranacogene dezaparvovec-drlb), a gene therapy for hemophilia B that is approved for adults who are on preventive treatment or have a history of life-threatening bleeding or repeated, serious bleeds that occur spontaneously.
A few experimental hemophilia gene therapies are currently being tested in clinical trials. These include:
- giroctocogene fitelparvovec for hemophilia A
- GS1191 for hemophilia A
- arvenacogene sanparvovec for hemophilia B.
Benefits and potential impact
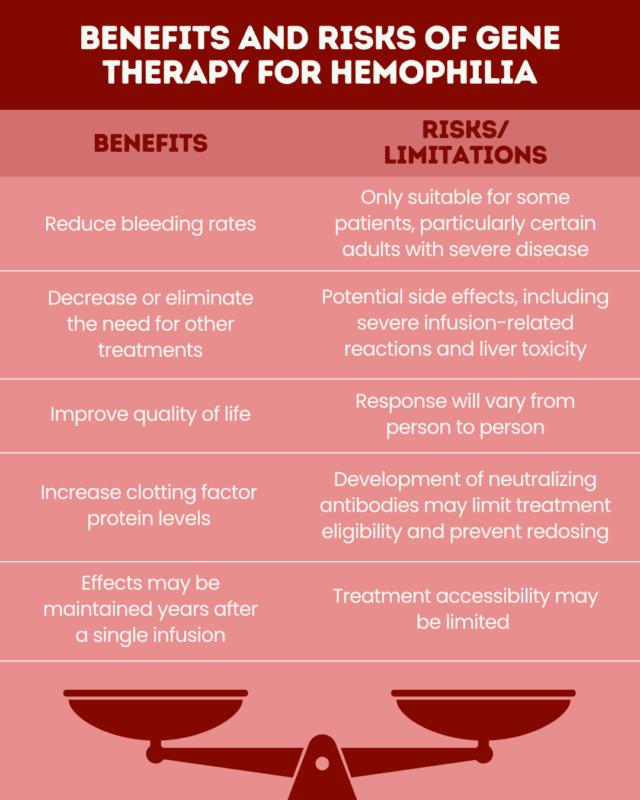
Available data indicate that gene therapy for hemophilia may:
- increase the levels of clotting factor proteins
- significantly reduce bleed rates
- decrease or eliminate the need for other treatments
- improve patients’ quality of life.
Research has shown these benefits can last for years after the treatment is administered. Sustained effects after four or five years have been reported in large clinical studies of Roctavian and Hemgenix. Some studies have reported benefits lasting more than a decade. However, because gene therapy is a relatively new, its long-term impact is not yet fully known. Scientists are actively working to collect data on the long-term benefits and potential risks of gene therapy.
Risks and limitations
As with any type of medical treatment, gene therapy comes with risks and the potential to cause side effects. Specific safety profiles vary from therapy to therapy, but some side effects reported with FDA-approved gene therapies for hemophilia include:
- headache
- infusion-related reactions
- fatigue and malaise
- elevated levels of creatine kinase, a marker of muscle damage
- elevated levels of liver enzymes, an indication of liver damage
- vomiting, abdominal pain, and/or flu-like symptoms.
Some of the more serious safety issues that may occur with gene therapies include:
- infusion-related reactions that can include serious allergic reactions
- liver toxicity, which may require close monitoring and specific treatment
- liver cancer, which may, in theory, arise if the viral vectors used in gene therapies insert themselves into a person’s DNA in a way that causes harmful genetic changes that promote uncontrolled cell growth.
In addition, there are some limitations and caveats to keep in mind about available gene therapies. First, each individual responds to gene therapy differently, which means that while gene therapy may be transformative for some people with hemophilia, other patients may not experience such pronounced effects.
Not everyone is eligible for these treatments, which are indicated specifically for certain adults with severe disease.
Gene therapies are costly, with Roctavian and Hemgenix costing millions of dollars, so access can vary considerably depending on factors such as insurance coverage and place of residence.
Gene therapies using viral vectors also have some noteworthy limitations because the body’s immune system will tackle the viral vector just like it does with any virus: by producing antibodies to neutralize the threat. Some people have pre-existing antibodies against the virus, which can stop the gene therapy from working correctly and limit treatment eligibility. Once the therapy is administered, the immune system will usually make neutralizing antibodies against the virus, so virus-based gene therapies generally cannot be given more than once.
Hemophilia News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Global survey finds many women with hemophilia face diagnostic gaps
- Learning how to infuse factor gave my family freedom, part 1
- Guest Voice: My sons with hemophilia are blessings after a devastating loss
- Love shows up to navigate hemophilia, distance, and family bonds
- We can find signs of calm in the storm if we remember to look