Hip replacement can benefit hemophilia patients, but risks exist
Study: Clinicians, patients need to be aware of potential for infection, bleeding
Written by |
Total hip replacement surgery for hemophilia patients is usually successful in creating a more functional joint, according to a systematic review study.
However, clinicians and patients need to be aware of potential risks, such as infection and bleeding.
“This paper confirms the findings of previous studies that [[total hip replacement surgery] is an effective treatment for advanced-stage haemophilic arthropathy, offering significant pain relief and improved function. However, its high rate of complications has to be reduced with a correct perioperative hemostasis [bleed control] and a good surgical technique,” researchers wrote.
The study, “Prosthesis survival situation and complications following total hip arthroplasty in hemophilic patients: a systematic review,” was published in BMC Musculoskeletal Disorders.
Hemophilia patients may have higher risk of complications
Hemophilia is characterized by abnormally easy and prolonged bleeding. People living with hemophilia often experience bleeding in the hips and other joints, which can cause damage. When damage to the hip joint becomes very severe, total hip replacement surgery may be recommended to help patients maintain mobility and life quality.
Hip replacement “has become nearly the only viable treatment option in advanced stages [of hemophilia-related hip joint damage], significantly alleviating pain and improving joint function,” the researchers wrote.
However, due to their underlying disease, people with hemophilia also may be at a higher risk of developing complications associated with hip replacement surgery.
To assess the outcomes of hip replacement surgery for people with hemophilia, scientists in China conducted a meta-analysis, which is a type of study that pools data from previous studies and analyzes it collectively. This meta-analysis included data from 14 studies published between 1986 and 2023.
“To the best of our knowledge, this is the first systematic review to comprehensively evaluate the outcomes of [total hip replacement] in patients with hemophilia, focusing on prosthesis survival and complications,” the researchers wrote.
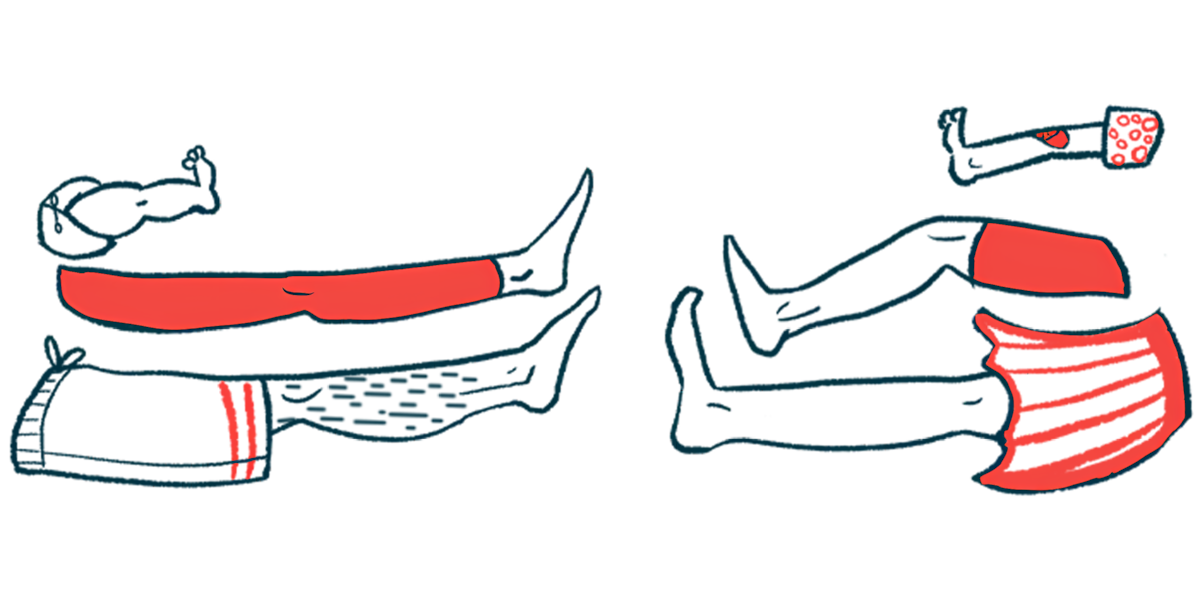
Prostheses survived in 175 out of 190 surgeries
Results showed that, out of 190 total hip replacement surgeries, 175 of the prostheses survived — in other words, the hip replacement procedure was successful in giving the patient a new, more mobile hip joint. Overall, the researchers said this reflects generally favorable outcomes. In the rare events where prostheses failed, this was due either to infections in the joint or to aseptic loosening, or inflammation around the implant that causes it to fail.
The researchers also reviewed major complications that were reported following hip replacement surgery in hemophilia patients. The most common ones were related to bleeding and anemia. Other complications included problematic clotting, abnormal bone growth, and poor wound healing.
“These findings underscore the importance of individualized perioperative management, including optimized clotting factor replacement, infection control, and advanced surgical planning,” the researchers wrote, noting that further research is needed to identify the best ways to minimize bleeding and manage other complications.
The scientists noted that the studies included in this meta-analysis were generally small and had variable designs. There also wasn’t enough data to conduct statistically robust analyses looking for factors that might affect outcomes, such as HIV status and treatment usage. As such, the scientists emphasized the need for further investigation into the outcomes following hip replacement in hemophilia, as having more data may help guide clinicians in coming up with strategies to optimize outcomes.
“By addressing prosthesis survival and complications, this review provides valuable insights for clinicians in preventing and managing complications following [hip replacement] in patients with hemophilia,” they wrote.