Could Relating Common Procedures to Pain Scales Help Patients?
Written by |
Many of us have been there. We’ve walked into a medical office in pain, seeking relief. As the doctor completes an evaluation, we are asked that common and potentially problematic question: “Please rate your pain on a scale of 1 to 10.”
I hate pain scales. Perhaps you loathe them as much as I do? I can’t stand them because they feel entirely subjective. Critically, they can lack a common understanding.
As someone who has lived with chronic pain for my entire life, pain scales seem useless, or at least ambiguous. During my youth, medical professionals thought girls could not get hemophilia. As a result, I was told for years that my pain was not real. To survive, I learned to ignore it. Ask anyone with hemophilia, and they will tell you that the pain is genuine. I had no choice but to carry on, and I developed an incredibly high pain tolerance.
When asked by a doctor to rate pain if, for example, I have a joint bleed, I find myself pausing. My “2” may be the doctor’s “7.” Without a universal language to describe your pain, it can be grossly misunderstood — or even worse, dismissed.
Finding commonality
I am thankful for a women’s breakout group at the Hemophilia Federation of America’s annual symposium earlier this year. One member of the group talked about the necessity of defining pain more clearly by identifying a commonality with which the medical provider can relate. An example might be, “Dr. Hemophilia, you are asking me to rate my pain. Have you ever had a wisdom tooth removed? When I had mine removed, I would rate that pain a ‘4.’ I am currently feeling knee pain at a ‘5.’” The doctor might regard the pain associated with having a wisdom tooth removed as a “6” or “7.” Relating pain levels to a common medical procedure is one way to minimize the misunderstandings associated with self-reporting using a scale.
The day after my hysterectomy, I asked the hospital to reduce my dose of painkillers to one quarter. My medical team advised me to stay on the lowest possible dose as they were concerned with keeping my pain under control. I explained to them that my pain level was tolerable, but the side effects of narcotic medications were not. I was down to an anti-inflammatory to treat my pain mere days after the surgery. And it was only then, when I demanded to reduce the painkilling medications, that my doctors fully understood my high pain tolerance.
Faces versus numbers
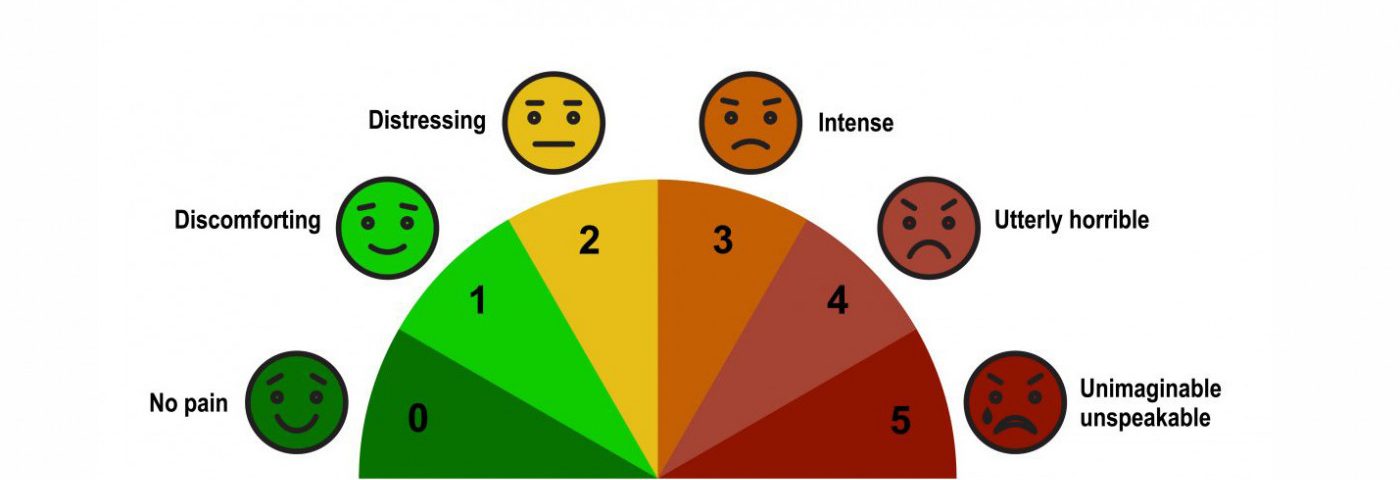
I would prefer to point at a pain scale with faces ranging from “happy” to “sad” than one offering a seemingly arbitrary number. I believe a connection to an expressive face has a greater chance of conveying my experience more accurately. Taking the time to establish the common language of similar pain experiences is likely to result in a better connection to, and understanding from, a health provider.
If you can relate to the realities of chronic pain, you might want to plan your next medical visit. Take time before your appointment to consider how you might establish a shared language of pain experiences with your doctor. As we develop these mutual understandings, we create more opportunities for improvements in our care.
***
Note: Hemophilia News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Hemophilia News Today or its parent company, Bionews Services, and are intended to spark discussion about issues pertaining to hemophilia.



Leave a comment
Fill in the required fields to post. Your email address will not be published.