FAQs about Altuviiio
There are no known interactions between Altuviiio and alcohol. However, because drinking alcohol while yaking certain medications can alter their effectiveness or cause side effects, patients who want to drink alcohol while on Altuviiio should discuss that with their healthcare providers.
By providing hemophilia A patients with a man-made version of factor VIII (FVIII), the blood clotting protein they are missing, Altuviiio should increase FVIII levels and reduce the frequency of bleeds. In the two Phase 3 clinical trials that supported its approval, the therapy significantly reduced the rate of annual bleeds by more than 70% when used as a preventive therapy, and helped resolve more than 90% of bleeds when used on demand.
In the XTEND-1 trial that supported Altuviiio’s approval, a significant reduction in the number of bleeds was observed in patients receiving prophylactic treatment after about one year. Moreover, when used as as on-demand treatment, a single dose of the therapy was sufficient to control 97% of the bleeds that occurred during the study. However, because each person is unique and can respond differently to a medication, patients are advised to talk with their healthcare team about how the therapy may help in their particular case.
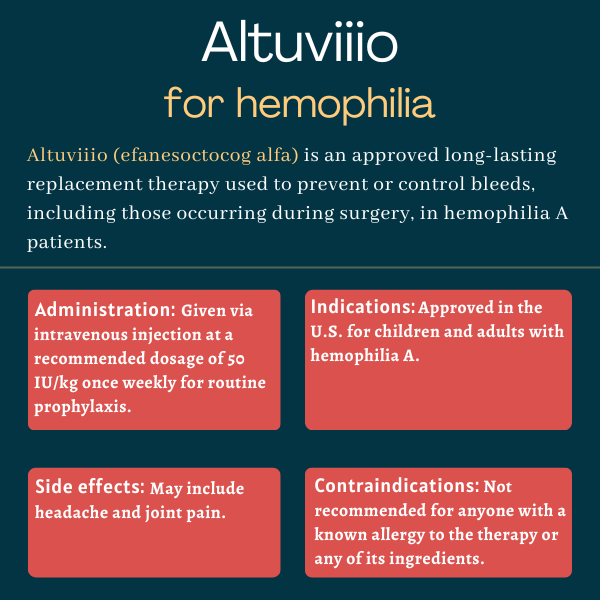
In clinical trials, the most common side effects of Altuviiio, reported in more than 10% of the patients, included headache and joint pain. Some patients reported back pain. Patients should ask their healthcare provider about these and other side effects that may be potentially experienced on the therapy.
The U.S. Food and Drug Administration (FDA) approved Altuviiio in 2023 for treating children and adults with hemophilia A. Altuviiio is specifically indicated as a routine prophylactic therapy to lower the frequency of bleeding episodes, as well as an on-demand treatment to control active bleeds, including those occurring during surgery.
Related Articles

 Fact-checked by
Fact-checked by