Qfitlia (fitusiran) for hemophilia
Last updated April 3, 2025, by Joana Carvalho, PhD

What is Qfitlia for hemophilia?
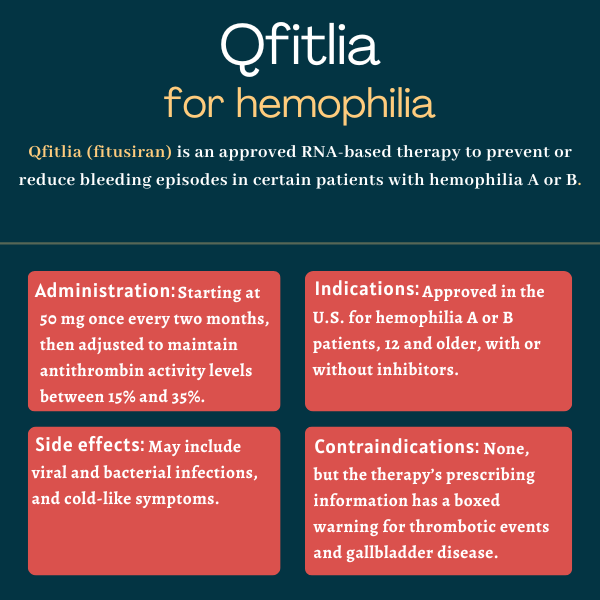
Qfitlia (fitusiran) is an RNA-based therapy that is approved in the U.S. to prevent or reduce the frequency of bleeding episodes in people with hemophilia A or B, with or without inhibitors, which are the neutralizing antibodies targeting the clotting factor they are missing.
The medication is administered via subcutaneous, or under-the-skin, injections that can be self-administered or given by caregivers after appropriate training. In 2018, Sanofi acquired global rights to develop and commercialize the therapy from Alnylam Pharmaceuticals.
Therapy snapshot
| Brand name: | Qfitlia |
| Chemical name: | Fitusiran |
| Usage: | Prevent or reduce the frequency of bleeds in people with hemophilia A or B |
| Administration: | Subcutaneous injection |
How does Qfitlia work in hemophilia?
Hemophilia is a rare condition in which blood cannot clot properly because a clotting protein is faulty or missing. In hemophilia A, patients have deficient levels of factor VIII (FVIII) due to mutations in the F8 gene. In turn, F9 gene mutations that affect the production or function of factor IX (FIX) are the cause of hemophilia B.
Due to the reduced levels of these clotting factors, people with hemophilia often experience prolonged bleeding episodes, either spontaneously or following an injury, that can be difficult to control.
Qfitlia is an RNA-based therapy designed to limit the production of antithrombin, a natural anticoagulant protein that inhibits multiple clotting factors.
The antithrombin protein is encoded by the SERPINC1 gene. When that gene is read, an intermediary molecule called SERPINC1 messenger RNA (mRNA) is made to be used by the cell’s protein-making machinery as a template for antithrombin’s production.
As a small interfering RNA (siRNA), Qfitlia works by binding to and promoting the degradation of SERPINC1 mRNA molecules, thereby interfering with the production of antithrombin and reducing its levels.
A particular feature of Qfitlia is that it contains a molecule called N-acetylgalactosamine attached to the siRNA molecule. This is meant to enable the therapy to be delivered directly to liver cells, which are the main producers of clotting factors in the body.
By limiting the production of antithrombin in the liver, Qfitlia is expected to improve the body’s ability to form blood clots. This may help prevent excessive bleeding in hemophilia patients, regardless of the presence of inhibitors against FVIII or FIX.
Who can take Qfitlia?
Qfitlia was approved by the U.S. Food and Drug Administration (FDA) in March 2025 as a routine prophylactic treatment to prevent or reduce the frequency of bleeds in individuals, 12 and older, with hemophilia A or B, with or without FVIII or FIX inhibitors — becoming the first and only therapy of its class to become available for this indication.
Who should not take Qfitlia?
Qfitlia’s prescribing information lists no contraindications to its use.
However, the therapy’s label has a boxed warning for thrombotic, or blood clot-related, events, as well as acute and recurrent gallbladder disease, which have occurred in patients treated with Qfitlia.
Patients should be closely monitored for signs and symptoms of thrombotic events and gallbladder disease. Treatment with Qfitlia should be interrupted for those experiencing a thrombotic event, and interrupted or discontinued for those developing gallbladder disease.
Qfitlia should also be avoided in patients with impaired liver function.
How is Qfitlia administered?
Qfitlia is given via subcutaneous injections that can be self-administered or given by caregivers after proper training from a healthcare provider. In the case of adolescents, it’s recommended the therapy be administered by an adult or under adult supervision.
The therapy comes in a clear, colorless to pale yellow solution. It is supplied in:
- a single-dose prefilled pen containing 50 mg of the therapy’s active ingredient (in 0.5 mL of solution)
- a single-dose vial containing 20 mg of the therapy’s active ingredient (in 0.2 mL of solution).
Injections are given into the thigh or abdomen (except for the 2 inches around the navel). Caregivers may inject the therapy in the outer portion of the upper arms. Injections should not be given in areas where the skin is tender, damaged, bruised, or scarred, or in regions with visible veins.
Qfitlia should be given at a starting dose of 50 mg once every two months. The therapy’s dose and dosing frequency should then be adjusted to maintain antithrombin activity between 15% and 35%.
Antithrombin activity should be checked before starting treatment and periodically thereafter using a companion test cleared by the FDA for that purpose. Qfitlia should not be started in patients in whom antithrombin activity levels are below 60%.
Antithrombin activity should be measured on the first, third, fifth, and sixth month after patients start receiving Qfitlia’s recommended starting dose or following any dose modification. In general, dose and dosing frequency adjustments are needed when:
- antithrombin activity is below 15%. In these cases, a dose reduction is required. The lower dose should start being given three months after the previous dose.
- antithrombin activity is above 35% after six months, or the patient has failed to attain adequate bleed control. In these cases, a dose escalation should be considered.
Once a patient’s target dose is identified, antithrombin activity should be measured annually. Additional measurements may be required in patients who fail to achieve adequate bleed control. If treatment with Qfitlia is stopped, patients no longer need to have their antithrombin activity checked regularly, unless they are bleeding and need treatment with a clotting factor concentrate or bypassing agent.
If a dose of Qfitlia is missed, the missing dose should be administered as soon as possible. Afterward, the patient’s usual dosing schedule should be resumed.
In the first seven days after starting on Qfitlia, patients may continue taking their previous preventive treatment (clotting factor concentrate or bypassing agent).
If breakthrough bleeds occur in the first seven days of treatment with Qfitlia, they can be managed using the same dose of the patient’s previous treatment. If they happen after seven days, they should be managed with a lower dose of the patient’s previous treatment to minimize the risk of blood clotting-related events.
Qfitlia may be stored at room temperature for up to three months or in the fridge. The therapy can be administered right away if stored at room temperature. If kept in the fridge, the therapy should be taken out of the fridge to reach room temperature for at least 30 minutes before being administered. Any unused portion of the medication should be discarded. The therapy should be kept away from direct heat and sunlight, and should never be frozen.
Qfitlia in clinical trials
The safety and efficacy of Qfitlia for individuals, 12 and older, with hemophilia A or B was established in two Phase 3 clinical trials.
- The ATLAS-INH (NCT03417102) trial enrolled 57 patients with inhibitors who previously received on-demand treatment with bypassing agents to control bleeds.
- The ATLAS-A/B (NCT03417245) trial enrolled 120 patients without inhibitors who were previously treated with a clotting factor concentrate on an on-demand basis to control bleeds.
Patients in these studies were randomly assigned to receive prophylactic treatment with Qfitlia at a monthly fixed dose of 80 mg, or to continue receiving on-demand treatment with a bypassing agent or a clotting factor concentrate for nine months.
Findings from the two trials indicated prophylactic treatment with Qfitlia significantly lowered annualized bleeding rates by 90% or more when compared with on-demand treatment in patients with and without inhibitors.
ATLAS-OLE extension study
A total of 227 patients who completed either of these two studies or another Phase 3 trial of Qfitlia, called ATLAS-PPX (NCT03549871), were eligible to enter a long-term extension study called ATLAS-OLE (NCT03754790) to continue treatment with Qfitlia.
While the therapy was initially administered at a monthly fixed dose of 80 mg in the extension study as in the previous trials, that was later changed in a protocol amendment in order to reduce the risks of thrombotic events, gallbladder disease, and liver toxicity, which were observed in patients given that dose.
Per the amendment, Qfitlia started being administered at a starting dose of 50 mg once every two months, with subsequent adjustments made to maintain antithrombin activity between 15% and 35%. A total of 213 patients subsequently transitioned to the revised dosing regimen in the extension study.
The efficacy of Qfitlia’s antithrombin dosing regimen was evaluated over the course of seven months in the extension study, following a six-month dose adjustment period. During that period, the median observed annualized bleeding rate for treated bleeds was 3.8 bleeds per year in patients without inhibitors and 1.9 bleeds per year in those with inhibitors.
Efficacy analyses based on antithrombin dosing regimen
Qfitlia’s approval was backed by efficacy analyses that compared data from patients who received the antithrombin dosing regimen in ATLAS-OLE with data from the two control on-demand treatment groups of ATLAS-A/B and ATLAS-INH.
Data from these studies showed that, compared with on-demand treatment with a clotting factor concentrate or bypassing agent, prophylactic treatment with Qfitlia reduced the annualized bleeding rate for treated bleeds by more than 70% in patients with and without inhibitors.
Specifically, in patients with inhibitors, the annualized bleeding rate for treated bleeds dropped from 19.1 bleeds per year with a bypassing agent in ATLAS-INH to 5.1 bleeds per year with Qfitlia in ATLAS-OLE. In those without inhibitors, the rate for treated bleeds dropped from 31.4 bleeds per year with a clotting concentrate in ATLAS-A/B to 9 bleeds per year with Qfitlia.
Annualized bleeding rates for treated spontaneous bleeds and for treated joint bleeds also dropped by more than 70% with Qfitlia prophylaxis compared with on-demand treatment in patients with and without inhibitors.
Other ongoing trials
Besides ATLAS-OLE, which is still ongoing, Sanofi is conducting another Phase 3 clinical trial called ATLAS-NEO (NCT05662319) to assess the long-term safety and efficacy of Qfitlia in adults and adolescents with hemophilia A or B, with or without inhibitors.
Also underway is the open-label ATLAS-PEDS trial (NCT03974113), which is assessing the safety and pharmacological properties of Qfitlia in boys ages 1 to 11 with severe hemophilia A or B who are positive for FVIII or FIX inhibitors. The primary goal is to measure blood activity levels of antithrombin over 256 weeks (nearly five years) of treatment. Secondary outcome measures include assessing the therapy’s safety and concentration in the blood.
Common side effects of Qfitlia
The most common side effects of Qfitlia reported in hemophilia patients include:
- viral infections
- bacterial infections
- cold-like symptoms.
Blood clot-related events
Qfitlia’s prescribing information carries a boxed warning for thrombotic events because serious blood clot-related events have occurred in treated patients. The risk of such events is higher in patients who:
- have persistent antithrombin activity levels lower than 15%
- have other coexisting conditions that increase their predisposition to thrombosis
- underwent surgery, and bleed management guidelines were not followed after the procedure
- have an indwelling venous catheter (a device to facilitate vein access for infusions)
- have received Qfitlia at a monthly fixed dose of 80 mg.
Antithrombin activity levels should be monitored with an FDA-cleared test, and Qfitlia dose adjustments should be made to ensure they fall within the range of 15% to 35% to minimize the risk of thrombosis.
Patients should also be monitored for signs and symptoms of blood clot-related events, and should seek immediate medical help if they experience any of the following signs and symptoms during or after treatment with Qfitlia:
- swelling, pain, or redness in the arms or legs
- coughing up blood
- shortness of breath
- severe chest pain or tightness
- fast heart rate
- feeling faint or passing out
- severe or persistent headache
- difficulty speaking or understanding language
- feeling confused
- numbness or weakness in the face, arms, or legs
- sudden loss or changes in vision, eye pain, or swelling.
Prophylactic treatment with Qfitlia should be interrupted if such an event occurs. The benefits and risks of resuming Qfitlia prophylaxis after a thrombotic event should be carefully considered.
Because hormonal contraceptives containing estrogen may increase the risk of blood clot-related events, patients are advised to use a non-hormonal form of birth control before and during treatment with Qfitlia.
Active and recurrent gallbladder disease
Qfitlia’s prescribing information carries a boxed warning for acute and recurrent gallbladder disease. The use of the therapy is associated with an increased risk of gallbladder disease, including gallstones and gallbladder inflammation, which may require surgery to remove the gallbladder.
Some patients on Qfitlia’s monthly fixed dose of 80 mg in trials underwent gallbladder removal surgery, with one patient also developing complications that included pancreatitis (pancreas inflammation) and cholangitis (inflammation of the bile ducts).
Patients should be monitored for signs and symptoms of gallbladder disease, and should contact their doctor if they experience any of the following symptoms:
- abdominal pain
- indigestion
- nausea and/or vomiting.
If gallbladder disease is suspected, appropriate imaging and clinical follow-up are recommended. Prophylactic treatment with Qfitlia may be interrupted or permanently stopped in patients developing gallbladder disease. Alternative hemophilia treatments may be considered in patients with a history of symptomatic gallbladder disease.
Liver toxicity
Elevations in the levels of liver enzymes — an indication of liver inflammation and/or damage — have occurred in patients treated with Qfitlia in clinical trials, particularly those receiving the monthly fixed dose of 80 mg. A case of moderate liver injury attributed to treatment has also been reported.
Qfitlia should be avoided in patients with impaired liver function. Lab tests to assess liver function should be conducted before patients start treatment, as well as on a monthly basis for at least six months after starting Qfitlia or after a dose increase, and periodically thereafter.
If new or worsening liver function abnormalities occur, appropriate medical management should be started, and lab parameters should be monitored until they return to normal. Qfitlia should be interrupted if liver enzyme levels are greater than five times the upper limit of normal.
The benefits and risks of resuming Qfitlia prophylaxis after liver enzyme levels return to normal should be carefully considered. Patients should permanently discontinue Qfitlia if they had restarted treatment and their liver enzyme levels again rise above five times the upper normal limit or they experience jaundice (yellowing of the skin) believed to be associated with liver toxicity.
Use in pregnancy and breastfeeding
No data are available on the use of Qfitlia in pregnant women, and no animal reproduction studies have been conducted. Thus, it is not known if Qfitlia can be harmful to a developing fetus when administered to a pregnant woman or whether it can affect reproductive capability. The prescribing information states the therapy should only be used during pregnancy if the benefits outweigh the potential risks, including those posed to the fetus.
It’s unknown whether Qfitlia can be passed into human milk, or its potential effects on nursing infants and milk production. When deciding whether or not to use the therapy during breastfeeding, the benefits of breastfeeding should be considered along with the mother’s clinical need for Qfitlia and any potential side effects to the nursing infant.
Hemophilia News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Related articles