Hympavzi (marstacimab-hncq) for hemophilia
Last updated April 1, 2025, by Joana Carvalho, PhD

What is Hympavzi for hemophilia?
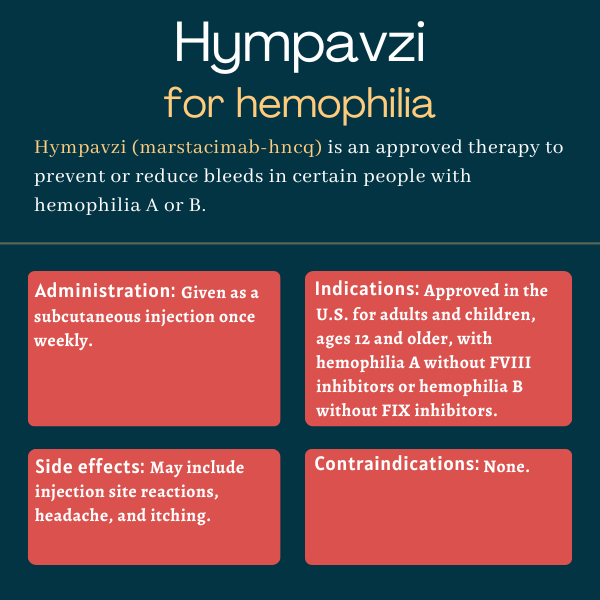
Hympavzi (marstacimab-hncq) is an antibody-based therapy that’s approved in the U.S. to prevent or reduce the frequency of bleeding episodes in adults and children with hemophilia A or B without inhibitors, or neutralizing antibodies targeting the missing clotting factor.
The therapy, developed and marketed by Pfizer, is administered once weekly via a subcutaneous, or under-the-skin, injection, which can be done by caregivers or patients following adequate training.
Therapy snapshot
| Brand name: | Hympavzi |
| Chemical name: | Marstacimab-hncq |
| Usage: | Prevention of bleeding episodes in hemophilia A or B patients |
| Administration: | Subcutaneous injection |
How does Hympavzi work?
In hemophilia, certain proteins needed for the blood to clot — specifically factor VIII, or FVIII, in the case of hemophilia A, and factor IX, or FIX, in hemophilia B — are either missing or dysfunctional. Lower than normal activity of these factors impairs blood clotting and causes patients to be more prone to excessive and prolonged bleeding, which can happen spontaneously or after a trauma or injury.
An antibody-based treatment, Hympavzi is designed to block the activity of an anticlotting protein called tissue factor pathway inhibitor, or TFPI. This protein normally helps prevent the formation of blood clots by preventing the generation of thrombin, a protein that plays a key role in the coagulation cascade.
By blocking TFPI and increasing thrombin generation, Hympavzi is expected to promote blood clotting through a mechanism that bypasses the need for FVIII or FIX, helping to prevent bleeds in people with either type of hemophilia, irrespective of inhibitor status.
Who can take Hympavzi?
Hympavzi was approved by the U.S. Food and Drug Administration (FDA) in October 2024 to prevent or reduce the frequency of bleeding episodes in adults and children, ages 12 and older, with hemophilia A without FVIII inhibitors or with hemophilia B without FIX inhibitors.
With the approval, Hympavzi became the first treatment for hemophilia A or B in the U.S. to be administered via a prefilled pen or syringe. It is also the first once-weekly subcutaneous injection therapy to become available for people with hemophilia B.
The therapy was also approved for a similar indication in the European Union in November 2024.
Who should not take Hympavzi?
According to Hympavzi’s prescribing information, there are no contraindications to its use.
How is Hympavzi administered?
Hympavzi is given as a subcutaneous injection, and is available in single-dose prefilled syringes or pens. These contain 150 mg of marstacimab, Hympavzi’s active ingredient, in 1 mL of a clear and colorless to light yellow solution.
The therapy is given at an initial loading dose of 300 mg (two 150 mg injections), followed by weekly 150 mg maintenance doses. Maintenance doses should be administered on the same day of each week, at any time of the day.
For patients weighing 50 kg (110 pounds) or more, and among whom bleeding control is considered to be inadequate, maintenance doses of 300 mg may be considered. Importantly, whenever more than one injection is required to administer a complete dose, each injection should be given in a different part of the body.
If a maintenance dose is missed, the skipped dose should be administered as soon as possible before the day of the next scheduled dose. Then, weekly dosing should be resumed with the same schedule or a new schedule based on when the missed dose was administered.
For patients on a maintenance dose of 150 mg, if more than 13 days have passed since the last dose was administered, a 300 mg loading dose should be given, followed by a 150 mg maintenance dose once weekly thereafter.
Hympavzi should be used under the guidance of a healthcare professional. The therapy may be self-administered by patients or given by caregivers, but always after proper training only.
Injections can be administered in the abdomen and thigh, or other sites if needed. Injections in the upper arm can be considered with a prefilled syringe and injections into the buttocks with a prefilled pen, but those should be performed exclusively by caregivers or healthcare professionals. Injection sites should also be rotated. Skin areas that are reddened, bruised, tender, hard, or scarred should be avoided.
Before starting Hympavzi, patients must discontinue treatment with any clotting factor products. Because Hympavzi has not been evaluated in the setting of major surgery, the therapy should be discontinued in patients undergoing such surgery and replaced by standard clotting factor products. A temporary interruption in Hympavzi treatment may also be considered for patients with acute severe illnesses, such as serious infections and trauma.
Hympavzi clinical trials
Hympavzi’s approval was supported by data from a Phase 3 clinical trial called BASIS (NCT03938792). That study enrolled 186 male children and adults, ages 12-74, with severe hemophilia A or moderately severe to severe hemophilia B, with or without inhibitors. The approval was specifically based on data from a subset of 116 patients without inhibitors.
BASIS trial
Before joining BASIS, participants entered a six-month observational period in which they received standard replacement therapies on a prophylactic (preventive) or on-demand basis to manage bleeds. After that period, all received prophylactic treatment with Hympavzi for about a year.
Participants were initially given a 300 mg subcutaneous loading dose, followed by 150 mg doses once weekly. Maintenance doses could potentially be increased to 300 mg after six months in patients weighing at least 50 kg and having two or more breakthrough bleeds.
The study’s main efficacy goal was to compare the annualized bleeding rate (ABR) for treated bleeds — the average number of bleeds requiring treatment per year — after one year of Hympavzi with that seen during the observational period. Other study goals included assessing the effects of Hympavzi on the incidence of spontaneous, joint, and total bleeds.
Results from the 116 patients without inhibitors showed that patients had a lower mean ABR for treated bleeds after switching to Hympavzi. Specifically, the 83 patients who received preventive replacement therapy during the observational period experienced a 35% reduction in the mean ABR for treated bleeds, with the number of yearly bleeds dropping from 7.85 to 5.08. Among the 33 who used on-demand replacement therapy, treated bleed rates fell by 92%, from 38 to 3.18 bleeds per year.
Hympavzi also was superior to on-demand replacement therapy and non-inferior to prophylactic replacement therapy in its ability to lower the incidence of spontaneous, joint, and total bleeds.
Data from an additional group of patients with inhibitors who are participating in BASIS are expected in 2025.
Other ongoing trials
Participants who complete the BASIS trial can enter an open-label extension study (NCT05145127) to continue receiving Hympavzi for up to seven years. Interim data from the extension study have suggested the therapy’s effect on bleeding rates is consistent over time.
Another ongoing Phase 3 trial called BASIS KIDS (NCT05611801) is testing Hympavzi in children with hemophilia as young as 1 year. The trial is open to children with severe hemophilia A or moderately severe to severe hemophilia B, with or without inhibitors, who have been on standard replacement therapy or bypassing agents for at least a year.
The trial aims to enroll about 100 participants. All will receive weekly subcutaneous injections of Hympavzi, with the goal of evaluating both its safety and its effect on bleeding rates after about one year. These results are expected in late 2028.
Common side effects of Hympavzi
The most common side effects reported in hemophilia patients treated with Hympavzi include:
- injection site reactions
- headache
- itching, known as pruritus.
Blood clots
Hympavzi may increase the risk of thromboembolic events, or blood clotting-related complications. Treatment should be interrupted if signs of thromboembolism occur and patients should be managed as clinically indicated.
Allergic reactions
Hympavzi may cause allergic reactions, including hives and pruritus. If a severe allergic reaction occurs, the therapy should immediately be discontinued and patients should promptly seek emergency treatment.
Use in pregnancy and breastfeeding
No data are available on the use of Hympavzi in pregnant women. However, based on the therapy’s mechanism of action and the fact that it can pass through the placenta, it’s believed that Hympavzi may be harmful to a developing fetus if used during pregnancy.
Pregnant patients should be informed of the potential risks to the fetus and women with reproductive potential should use effective contraception during Hympavzi treatment and for at least two months after their last dose. Female patients with reproductive potential should also take a pregnancy test before starting treatment.
There are also no data on the presence of Hympavzi in human milk and its potential effects on nursing infants and milk production. Patients are advised to discuss with their care team the potential benefits and risks of using Hympavzi while breastfeeding.
Hemophilia News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Rehab improves knee replacement outcomes in hemophilia patients
- Navigating grief as the parents of children with chronic illness
- Sometimes changing doctors is not only unavoidable, but vital
- The extra cargo of college life that’s putting my son in the driver’s seat
- Altuviiio safe, effective in patients with severe hemophilia A: Study
Related articles