Hemophilia causes
Hemophilia, a disorder characterized by excessive bleeding, is caused by the lack of activity of certain clotting factors, which are proteins that are needed to form blood clots.
Most cases of hemophilia are the result of mutations in a gene that provides instructions for making a specific clotting factor protein. As a consequence of these mutations, people with hemophilia either produce a faulty version of the clotting factor, too little of it, or none at all. In the majority of cases, these mutations are inherited and the disease is present from birth. These forms of the disease are sometimes referred to as congenital hemophilia.
Mutations in different genes cause different types of hemophilia:
- Mutations in F8, the gene that provides instructions for making clotting factor VIII, cause hemophilia A, which is also known as classic hemophilia.
- Mutations in F9, the gene that encodes for clotting factor IX, cause hemophilia B, which is also known as Christmas disease.
- Mutations in F11, the gene that provides instructions to make clotting factor XI, result in hemophilia C, also referred to as Rosenthal disease.
Testing for these mutations and consequent low levels of clotting factors is used in the diagnosis of hemophilia.
Hemophilia inheritance
In the majority of cases, hemophilia is caused by mutations that a person inherits from their biological parents. The specific hemophilia inheritance pattern differs depending on the disease type.
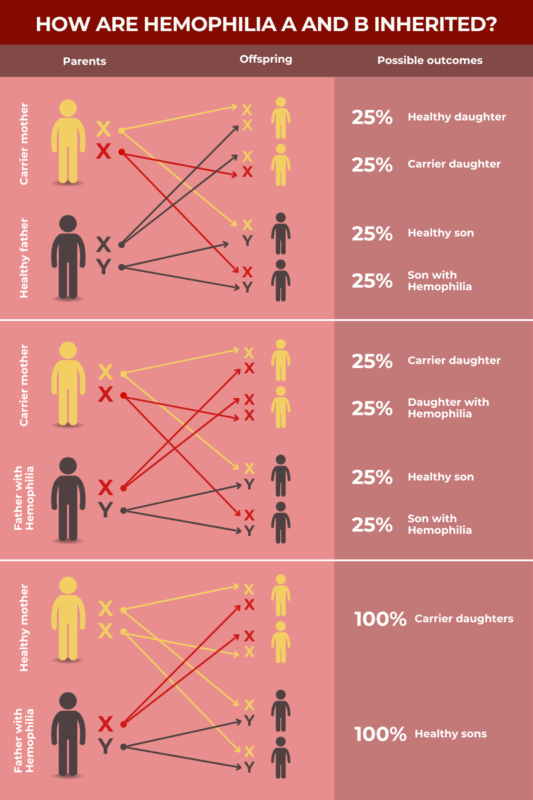
Inheritance of hemophilia A and B
The F8 and F9 genes, which are implicated in hemophilia A and B, respectively, are both located on the X chromosome, which is one of the two sex-determining chromosomes. Girls have two X chromosomes, while boys have one X chromosome and one Y chromosome.
One working copy of F8 or F9 is sufficient to allow for the production of clotting factors. As such, female individuals who have a mutation on one X chromosome usually don’t develop severe hemophilia, as long as there’s a functional version of the gene on their other X chromosome. Consequently, hemophilia A and B affects mainly boys.
Female individuals who carry one mutated copy of F8 or F9, and a second healthy copy, are referred to as carriers, since they don’t usually have overt hemophilia symptoms, but can still pass the disease-causing mutation on to their children.
If a female carrier for hemophilia A or B has a child with someone who does not have hemophilia, there is a:
- 25% chance the child will be male and have hemophilia.
- 25% chance the child will be male and not have hemophilia.
- 25% chance the child will be female and a carrier.
- 25% chance the child will be female and not be a carrier.
If a female carrier for hemophilia A or B has a child with someone who also has the same type of hemophilia, there is a:
- 25% chance the child will be male and have hemophilia.
- 25% chance the child will be male and not have hemophilia.
- 25% chance the child will be female and have hemophilia.
- 25% chance the child will be female and a carrier.
If a male individual with hemophilia A or B has a child with someone who is not a carrier, then all their male children will not have hemophilia, but all of their female children will be carriers.
Inheritance of hemophilia C
Unlike the F8 and F9 genes, the F11 gene that is implicated in hemophilia C is not located on the X chromosome. Instead, it’s found on chromosome 4. Every person inherits two copies of the F11 gene, irrespective of their biological sex.
In most cases, hemophilia C is inherited in an autosomal recessive manner, which means the disease will develop only if both copies of the F11 gene are mutated. People with only one mutated copy are said to be carriers, because they won’t have overt symptoms of the disease, but can still pass the mutation on to their biological children.
If two hemophilia C carriers have a child, there is a:
- 25% chance the child will have hemophilia C.
- 50% chance the child will be a carrier.
- 25% chance the child will not have hemophilia C or be a carrier.
More rarely, some cases of hemophilia C are inherited in an autosomal dominant manner, meaning that only one mutated copy of the F11 gene is sufficient to cause the disease. If someone with this subtype of hemophilia C has a child, there is a 50% chance of passing on the disease-causing mutation.
Spontaneous mutations
Although most mutations that cause hemophilia are inherited from an individual’s biological parents, it’s possible for mutations to arise spontaneously, or de novo, in a child without a family history of hemophilia. These mutations account for roughly a third of the cases of hemophilia A and B.
These mutations arise mainly due to errors in DNA replication that occur in the early development of sperm or egg cells. As a consequence, these reproductive cells may harbor mutations that aren’t found in the rest of the body, but can still be passed on if those cells end up being used to conceive a child.
Other causes
In very rare cases, in approximately 1.5 in a million people, a malfunction in the immune system can lead to the onset of an acquired form of hemophilia.
The immune system normally produces proteins called antibodies that latch onto viruses, bacteria, and other disease-causing agents that could harm the body. When an antibody binds to its target, it triggers reactions leading to the destruction of those invaders. In autoimmune diseases, however, the body mistakenly produces antibodies that target healthy parts of the body itself.
In the case of acquired hemophilia, the body attacks its own clotting factors, usually factor VIII, whose deficit causes hemophilia A. This reduces the amount of clotting factor available to effectively promote blood clot formation and prevent bleeds.
It’s not known what exactly causes acquired hemophilia to develop. In roughly half of the cases, this rare form of hemophilia arises in association with underlying illnesses, including other immune disorders, cancer, certain skin conditions, and pulmonary diseases.
Risk factors
Most cases of hemophilia are caused by genetic mutations that are passed from parents on to their biological children. In these cases, the main risk factor is having a family history of the disease. For people with this family history who want to have biological children, genetic testing and counseling can help to inform their decisions.
The genes that cause the most common forms of hemophilia, types A and B, are located on the sex-determining X chromosome. Consequently, these forms of hemophilia disproportionately affect boys. Thus, being male is considered a key risk factor for hemophilia. Rarer types, namely type C and acquired hemophilia, affect people of both sexes at roughly equal rates.
In acquired hemophilia that is caused by a malfunction of the immune system, one of the main risk factors is age, since this disease type occurs mainly in the latter decades of life. Acquired hemophilia can also arise in people who have other underlying health problems, such as other autoimmune diseases or cancer. It can also occur as a complication following pregnancy and childbirth.
For people with hemophilia, some factors can increase the risk of bleeds. The most obvious is physical injury, so activities that have an elevated risk of injury, such as intense contact sports, can pose a high bleed risk. Certain medications, including some antibiotics, blood thinners, and anti-inflammatory medicines like ibuprofen, may increase the risk of bleeds as well.
A deficiency of vitamin K can cause excessive bleeding, particularly in infants. Supplements of this vitamin may be recommended for some people with hemophilia.
Hemophilia News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Rehab improves knee replacement outcomes in hemophilia patients
- Navigating grief as the parents of children with chronic illness
- Sometimes changing doctors is not only unavoidable, but vital
- The extra cargo of college life that’s putting my son in the driver’s seat
- Altuviiio safe, effective in patients with severe hemophilia A: Study
Related articles

 Fact-checked by
Fact-checked by