Switching to Elocta Helps Reduce Hem A Joint Bleeds in France
People in France with severe hemophilia A who switched to Elocta (efmoroctocog alfa) — an extended half-life replacement therapy — had fewer infusions and a reduced rate of joint bleeds, a real-world study reports.
Notably, those who switched to Elocta had a higher bleeding rate, including joint bleeds, before switching. In contrast, patients who remained on standard short half-life therapies showed no changes in their bleeding rates.
These findings may help patients diagnosed with the bleeding disorder make informed decisions about their treatments, giving them a better understanding of the benefits of each option, researchers say.
The study, “rFVIII-Fc in severe haemophilia A: the incentive switch in case of high risk of joint bleedings,” was published in the European Journal of Clinical Investigation.
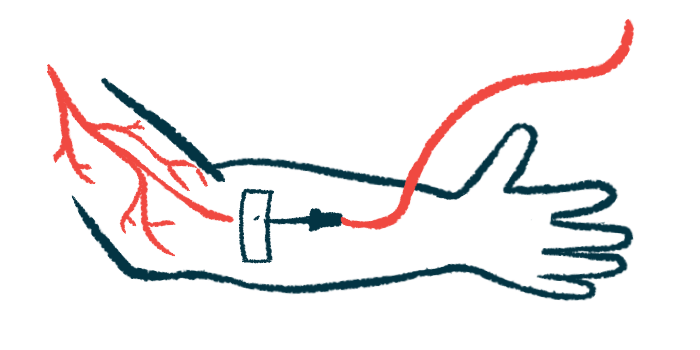
One of the standard treatments to prevent or stop bleeds in hemophilia A is replacement therapy. It involves supplying a version of blood clotting factor VIII (FVIII), which is missing or defective in people with the condition.
Recently, extended half-life replacement therapies have become available. They are modified to increase the time they remain active in the body, resulting in fewer infusions without affecting clinical efficacy.
However, there remains a lack of real-world data on patients with severe hemophilia A who switched to extended half-life products from standard short half-life therapies in France.
MOTHIF-II (NCT03596814) was an observational study conducted at multiple sites across France. Here, researchers investigated the use of replacement therapy and the annual bleeding rates (ABR) in severe hemophilia A patients before and after switching to extended half-life replacement therapy.
Efmoroctocog alfa was the extended half-life therapy examined. It is sold as Elocta in Europe, and as Eloctate in the U.S. and Canada, among other countries. The medicine contains a lab-made formulation of FVIII attached to an Fc protein, in order to last longer in the body.
The study — which was funded by Sobi, a partner with Biogen in developing and marketing the therapy worldwide — covered two one-year periods: T1, spanning from July 2015 to June 2016; and T2, spanning from July 2017 to June 2018. In between, a one-year window gave patients sufficient time to consider switching treatment.
Therapy use was measured using prescription data from 156 severe hemophilia A patients who received preventive, or prophylactic, treatment during T1 and T2 and who did not have inhibitors — neutralizing antibodies against the lab-made FVIII. Bleeding rates were assessed in 83 of these patients with a measurable ABR.
Overall, a drop from three to two injections per week was seen in patients who switched to efmoroctocog alfa between T1 and T2, compared with those who remained on short-half-life therapy and maintained the same weekly injection frequency.
At the end of the study period, 85 participants (54.5%) switched to efmoroctocog alfa. From these, 48 (30.8%) switched between T1 and T2, and 37 (23.7%) during T2. No occurrence of inhibitors was reported during the study.
Compared with T1, the proportion of patients receiving twice-weekly injections rose by 28.0% in T2, while that of those receiving three injections per week decreased by 37.7%.
Of the 53 patients initially treated with three injections per week, 33 switched to efmoroctocog alfa, and among these, 23 (70%) reduced treatment frequency to two twice-weekly infusions. In comparison, 20 participants kept short-half life FVIII, with two (10%) changing to two injections per week.
Among the 120 participants with dispensed prescriptions, the mean amounts of FVIII used dropped significantly in T2 relative to T1. For those who switched to efmoroctocog alfa only, mean FVIII doses dropped from 4,333 to 3,921 IU/kg/year. In participants treated with short-half-life FVIII only, the mean amounts fell from 4,162 to 3,942 IU/kg/year.
At the end of the study, mean amounts of FVIII prescribed for prophylaxis were similar among those treated with short-half-life or extended half-life FVIII (3,942 vs. 3,921 IU/kg/year).
Of the 83 people with ABR data, 17 had no bleeds in both T1 and T2. The remaining 66 had 641 bleeding episodes (351 during T1 and 290 during T2). Joint bleeds occurred in 35.9% of the patients, while 19.2% experienced localized bleeding (hematomas), and 16.8% reported pain.
Although bleeding types were identical in T1 and T2, regardless of FVIII therapy, the initial bleeding profile was different between the two patient groups. Patients treated with efmoroctocog alfa only during T2 had a higher rate of joint bleeds during T1 than those given short-half-life FVIII only (52.0% vs. 30.6%). The ABR was about two times higher in patients who switched treatment compared with those who did not (6.4 vs. 3.0).
“The patients switched to [efmoroctocog alfa] had therefore a more ‘bleeder’ phenotype [characteristics] during T1 than patients left on standard FVIII,” the researchers wrote.
However, only patients who switched to efmoroctocog alfa saw their mean ABR drop significantly between T1 and T2 (6.4 to 4.0). The amounts of FVIII needed were also lower, dropping from 451 to 258 IU/kg/year/patient.
In comparison, individuals left on short half-life therapies had a similar ABR across T1 and T2 (3.0 vs. 3.2), with no differences in FVIII amounts.
Last, the researchers reported the mean joint ABR was the same for those left on short half-life FVIII between T1 and T2 (0.9 vs. 0.8), whereas it decreased in patients who switched (3.3 vs. 1.9), “consistent with the idea of a more ‘bleeder’ profile in switched patients.”
“Our evaluation is the first to report a peculiar profile of bleeding episodes in switched [severe hemophilia A patients], with a higher initial ABR caused by a clear predominance of [joint bleeds],” the team wrote. “This also suggests that the switch to [efmoroctocog alfa] may have been preferentially proposed to this particular profile of outpatient.”
“This study can therefore support shared decision-making and informed patient education, granting patients to better understand the benefits of each option and to express their preferences,” they wrote.