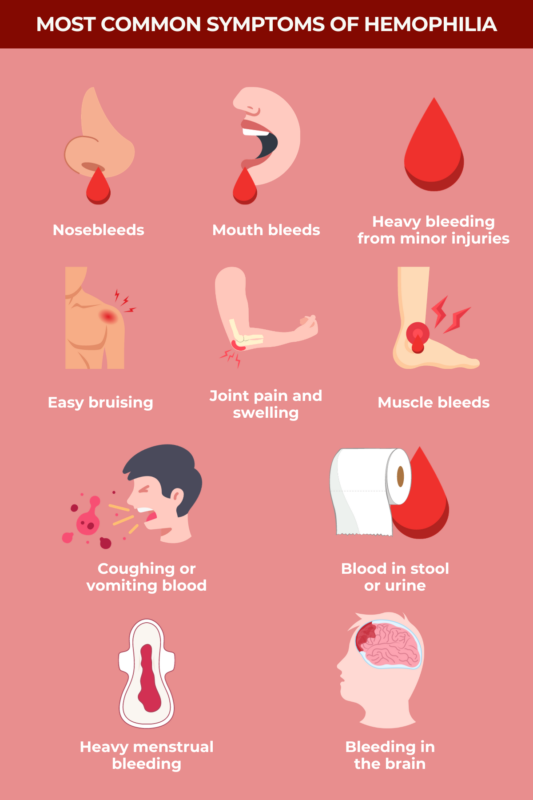
Hemophilia symptoms
Hemophilia is a rare disorder characterized by excessive, prolonged bleeding episodes. Other common hemophilia symptoms include bruising, joint and muscle problems, and chronic pain.
People with hemophilia don’t produce enough of certain clotting factors, or proteins needed to produce the blood clots that help slow and stop bleeding after an injury. These deficiencies increase the risk of bleeding outside the body (external bleeding) or within the body (internal bleeding), which can lead to life-threatening blood loss and other serious complications.
Recognizing the signs of hemophilia is important to ensure timely diagnosis and prompt treatment that can prevent or control bleeds.
Excessive bleeding and bruising
Easy and excessive bleeding and bruising are the primary symptoms of hemophilia.
When a healthy person gets a cut, undergoes surgery, or bumps into something hard enough to cause bruising, the body recruits clotting factors to the injury site. These slow and then stop the bleeding. Without enough functional clotting factors, people with hemophilia bleed more easily than others or for longer after similar injuries.
Hemophilia severity is generally classified based on the activity of the affected clotting factor:
| Classification | Clotting Factor Activity | Characteristics |
|---|---|---|
| Mild | More than 5% but less than 40% of normal activity | Bleeds occur more easily after minor injuries or medical procedures |
| Moderate | 1% to 5% of normal activity | Bleeds often occur after injury, but may occasionally occur without an obvious cause |
| Severe | Less than 1% of normal activity | Bleeds occur after injury, but also commonly happen without a clear cause |
The main difference between mild, moderate, and severe hemophilia symptoms is the circumstances most likely to prompt bleeds. People with mild and moderate hemophilia primarily experience abnormal bleeding following an injury or surgery. Some people with moderate hemophilia may also occasionally experience spontaneous bleeding, which occurs without an obvious cause. These forms of the disease may not be diagnosed until later in childhood or adolescence.
By comparison, individuals with severe hemophilia may frequently experience spontaneous bleeds, which can start before birth or in the first few months of life.
There are two broad categories of bleeds in hemophilia: external and internal.
External bleeding
External bleeding in hemophilia is typically frequent and excessive, and can occur after small injuries or spontaneously. Common forms of external bleeding in hemophilia include:
- frequent and unexplained nosebleeds (epistaxis)
- heavy bleeding from small wounds or wounds that previously stopped bleeding
- unusual bleeding following injections or circumcision
- unexplained bleeding from the mouth or gums, or excessive blood loss after dental procedures
- heavy menstrual bleeding
Without medical attention, a simple cut can be dangerous for people with hemophilia, particularly in more severe forms, so prompt medical care is important.
Internal bleeding
Easy and excessive bruising, the result of internal bleeding just below the skin, is a common hemophilia symptom. Unexplained bruising when a child first begins to walk or crawl is often among the early signs of hemophilia in babies.
People with hemophilia may also experience other types of internal bleeding, including:
- bleeding into the joints, or hemarthrosis
- muscle bleeds
- bleeding in internal organs such as the liver, spleen, and kidneys
- bleeding in the chest and throat
Hemarthrosis is the most common type of bleeding in hemophilia, particularly in severe forms of the disease. It most often affects the knees, elbows, ankles, hips, wrists, and/or shoulders, and is more common among those who are most physically active. Bleeding into muscles is also relatively common, affecting 10% to 20% of hemophilia patients, and can cause significant blood loss. Muscle and joint bleeding in hemophilia may cause pain, swelling, and impaired mobility.
Other possible internal bleeding symptoms in hemophilia include:
- stomach pain
- swelling, rigidity, or tenderness in the abdomen
- blood in the stool, which may appear reddish or unusually dark and sticky
- blood in urine
- vomiting blood
- chest pain
- shortness of breath or difficulty breathing
- coughing up blood
Internal bleeding elsewhere may also cause symptoms related to the affected area. For example, bleeding near the eye can disrupt vision, and bleeding in the spine can cause back pain.
Regardless of where internal bleeding occurs in the body, patients may experience symptoms such as an abnormally fast heartbeat, rapid breathing, and low blood pressure.
Bleeding in the brain
Bleeding in the brain, also called intracranial bleeding or intracranial hemorrhage, is a serious type of internal bleeding and a leading cause of death in hemophilia. However, the risk of brain bleeds has decreased with modern preventive therapies.
The brain has many blood vessels that supply the nutrients and oxygen it needs to function. When these vessels rupture and bleed, patients may experience symptoms like:
- prolonged headache
- frequent vomiting
- sleepiness or low energy
- double vision
- weakness
- convulsions or seizures
Brain bleeds are more common in severe hemophilia. Children younger than 2 are at higher risk than older children, and using assistive birthing techniques like forceps or vacuums during delivery can increase the risk of intracranial bleeding in newborns.
Adults older than 60 with hemophilia also have a higher risk of brain bleeding, particularly if they have high blood pressure.
Complications
There is a range of hemophilia complications that may occur as a consequence of hemophilia and its treatment. Complications of joint bleeds may include:
- irreversible joint damage, called hemophilic arthropathy
- chronic joint pain
Hemophilic arthropathy is characterized by pain and reduced mobility in the affected joint. Hemophilia joint pain may affect around 75% of people with the disease at some point. Joint problems and reduced mobility can also contribute to weak, fracture-prone bones.
Complications of muscle bleeds may include:
- low levels of oxygen in the blood (anemia)
- unsteady blood pressure
- pain and swelling
- numbness, tingling, and other unusual sensations
Anemia and blood pressure changes are common when bleeds involve large muscles, leading to substantial blood loss. Bleeding into smaller, confined muscles, such as those in the calf and forearm, can lead to compartment syndrome, where increased pressure around a muscle causes swelling and pain. Unusual sensations may occur if the affected muscles swell and compress nerves.
The therapies used to manage hemophilia can also lead to certain treatment-related complications, including:
- inhibitors: People using factor replacement therapies, which provide the body with the missing clotting factor, may develop antibodies against that clotting factor. This can lead to hemophilia treatment not working as well as it should to control bleeds.
- blood-borne diseases: Historically, some hemophilia treatments were made using donated blood, increasing the risk of blood-borne diseases like hepatitis and HIV. However, with modern risk-minimizing programs in place, this is now extremely rare.
Do carriers of hemophilia have symptoms?
The most common forms of hemophilia — hemophilia A and B — are related to genes on the X chromosome, one of the two sex-determining chromosomes in humans. Males are mainly affected by hemophilia because they have only one X chromosome. If they inherit a disease-causing mutation, they don’t have another copy of the gene to compensate for its loss.
Females have two X chromosomes, so there is a greater likelihood that even if one copy is mutated, the other will be functional, allowing them to produce some working clotting factor. Females with one disease-causing mutation are called carriers. They don’t usually develop overt hemophilia, but can still pass the mutations to their biological children.
However, carriers can still experience unusual bleeding-related symptoms, particularly if they have low clotting factor activity. Symptoms of hemophilia in female carriers can include:
- heavy periods or other irregularities in menstruation
- frequent bruising
- frequent nosebleeds
- excessive bleeding following an injury, surgery, or childbirth
- bleeding in the mouth
Hemophilia News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
 Fact-checked by
Fact-checked by